Cervical internal carotid artery pseudoaneurysms (PA) are most commonly noted after trauma, but also occur secondary to mycotic infection, following cancers of the head and neck, and as a surgical complication. A Pipeline flow diversion device deployed across the PA neck, stabilized by a tunneled conventional carotid stent within a post endarterectomized carotid bifurcation, with successful occlusion of the PA has to our knowledge not been reported.
CASE REPORT
A 74-year male with a past medical history of hypertension, hyperlipidemia, and abdominal aortic aneurysm underwent routine carotid ultrasound testing that showed high-grade stenosis of the right internal carotid artery. A CT angiogram (CTA) showed greater than 95% stenosis with complex atheroma of the right internal carotid artery. The patient underwent an uneventful right internal carotid artery endarterectomy with a saphenous vein graft patch. The patient tolerated the procedure well and was discharged home on postoperative day one. Routine follow-up at 1 month and 6 months showed the patient to be doing well with no new symptoms and no transient ischemic attacks (TIA) or strokes. Physical examination at those times also noted no abnormalities of the incision site or at the patient's neck.
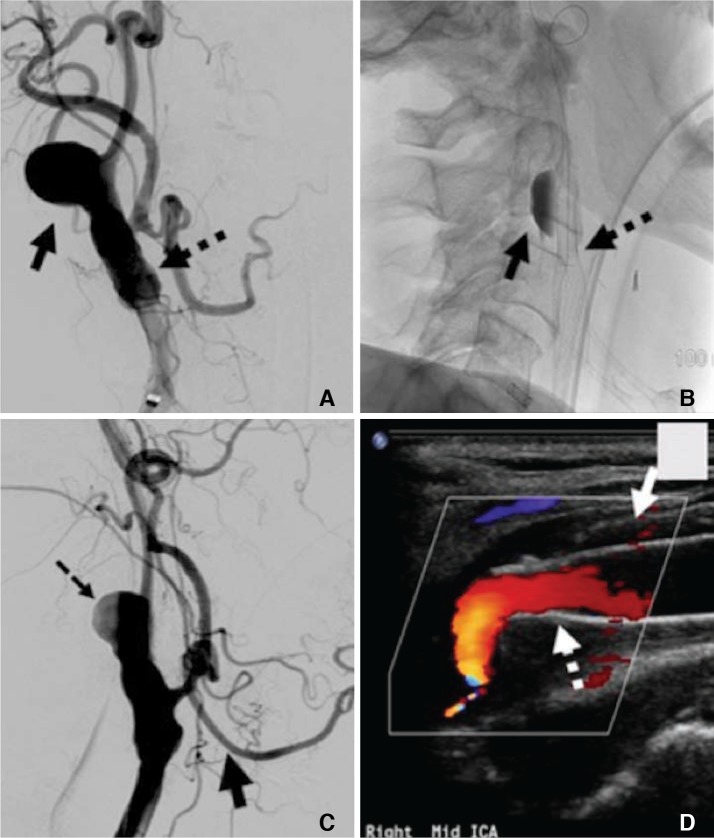
The patient noticed a painful enlarging pulsatile mass in the right inferior mandibular region 8 months after the endarterectomy. He had no symptoms of dysphagia, neck stiffness, blurred vision, dizziness, speech difficulty, or weakness. He exhibited no new symptoms of TIA or stroke. CTA of the head and neck demonstrated a broad neck pseudoaneurysm measuring 18 mm in widest dimension arising from the distal endarterectomy anastomotic site, just inferior and deep to the right mandibular angle (Fig. 1A, B). Dual flow diversion embolization device tunneled within a carotid stent implantation across the pseudoaneurysm neck was considered after a detailed discussion with the patient. Pre-procedural clopidogrel 75 mg and aspirin 325 mg daily for f ive days was commenced with appropriate P2Y12 platelet inhibition testing.
The procedure was performed under endotracheal general anesthesia. Using standard Seldinger technique access the right common femoral artery, diagnostic angiography the right common carotid artery revealed a laterally projection broad neck 18 mm×16 mm×12 mm pseudoaneurysm with marked disparate caliber of the extra-cranial carotid artery proximal and distal to the endarterectomy graft site (Fig. 2A). Using a 6F Inf inity sheath (Stryker, Freemont, CA, USA) a Marksman catheter (ev3 Inc. Menlo Park, CA, USA) was advanced through to the distal aspect of the right cervical internal carotid artery, distal to the pseudoaneurysm. A 5 mm×35 mm Pipeline embolization device (PED) (ev3 Inc.) was delivered across the PA neck with the distal aspect tethered within the normal caliber distal right cervical internal carotid artery at the distal endarterectomy anastomotic site. The proximal end of the PED remained free floating in the endarterectomized lumen, over the retained device delivery wire. The pipeline embolization device delivery catheter was then advanced through the implanted PED, distal to the aneurysm over the Pipeline device delivery wire. The delivery wire was then removed. A Synchro 14 exchange length microguidewire was advanced through the Pipeline delivery catheter, with subsequent removal of the delivery catheter. Implantation of an 8 mm–10 mm×40 mm Xact carotid stent (Abbott Laboratories, Abbott Park, IL, USA) over the exchange length Synchro 14 microguide wire within distal lumen of the already placed pipeline embolization device was performed, to anchor the distal end of the PED. The dual device construct approximated the disparate calibers of the carotid artery distal and proximal to the endarterectomy segment. Post dual stent placement angiography of the right common carotid artery revealed satisfactory flow through to the right distal cervical internal carotid artery with signif icant stasis within the pseudoaneurysm (Fig. 2B). The patient was discharged from the hospital on post-procedure day two with Plavix 75 mg daily for one year and Aspirin 325 mg daily for life. A follow-up at three months showed complete clinical resolution of the neck pain and mass with carotid sonography demonstrating complete resolution of the pseudoaneurysm (Fig. 2C, D).
DISCUSSION
Carotid artery PA following carotid endarterectomy (CEA) is rare. Literature reviews report this complication occurring in approximately 0.3%–0.6% of cases.1 Abdelhamid et al. reported this complication to be more common when a synthetic patch graft is used when compared to primary closure or a vein patch.2 PAs of the internal carotid artery distal to the endarterectomy anastomotic site are very rare.4 PA after CEA has a broad temporal distribution of occurrence, having been reported to develop days to many years following surgery.2 The pathophysiology of PA formation has been reported to be due to suture degeneration, infection, clamp induced damage, and shunt use.4
Varied surgical and endovascular approaches have been employed to treat cervical carotid PA. Open carotid surgery in the previously operated neck is both technically demanding and can lead to increased rates of complications for stroke and wound infection even in the most experienced hands.3 Additionally, open repairs may require subluxation of the mandible, obtaining proximal and distal control around large aneurysms, and carry a cranial nerve injury rate of 6–44%.5
Endovascular treatment for post carotid endarterectomy PAs provides a valid alternative to reoperation open surgery. Stent exclusion of the PA is the most common form of endovascular treatment. Types of stents reported in the literature include covered stents, bare metal stents, and vein-covered stents.5 Furthermore, the addition of coil embolization with coils being placed directly into the PA and stenting across the native carotid artery has also been reported with success.5 Holder et al. reported injecting thrombin directly into the PA with successful obliteration of a traumatic PA.6 Multiple, overlapping stents have also been reported in treatment of carotid PA, after endarterectomy and for traumatic PA.4,7 Benndorf et al. reported an overlapping covered stent technique for treatment of a dissecting traumatic carotid PA with adequate obliteration.7
The development of flow diversion for a variety of intracranial vascular pathologies has been widely studied. Nelson et al. reported an occlusion rate as high as 93.3% for the treatment of intracranial aneurysms with the PED.8 PED deployment has also been successfully used for treatment of iatrogenic injury to the internal carotid artery during sphenoid sinus surgery, as well as for traumatic carotid PA formation.9 The PED consists of 48 platinum and cobalt-nickel alloy strands in braided mesh design with pore sizes ranging from 0.02 to 0.05 mm and a metal area coverage between 30% and 35%.10 This metal area coverage provides the flow diversion properties of the device, and allows for pseudoaneurysm closure when positioned across the neck.10 The flow diversion device is available in a maximal width of 5 mm and can therefore not be positioned independently across a patulous endarterectomy site, hence the requirement of a 10 mm width overlapped conventional carotid stent to approximate the proximal and distal disparate calibers of the vasculature proximal and distal to the pseudoaneurysm.
To our knowledge dual PED and conventional carotid stent placement for successful treatment of PA following CEA has not been reported. The combined PED conventional carotid stent construct allows for restores the vessel lumen across the pseudoaneurysm and endarterectomy segment. This resolves the aneurysmal component without residual mass effect that would remain if intraluminal coils were placed.