 |
 |
- Search
| Neurointervention > Volume 17(3); 2022 > Article |
|
Abstract
Purpose
The purpose of this study was to evaluate trends in medical costs and prognosis in acute ischemic stroke (AIS) patients in Korea from 2008 to 2017 using medical claims data.
Materials and Methods
All data for the past decade was collected from a big data hub provided by the Health Insurance Review & Assessment Service. Using several Korean Standard Classification of Disease codes, we estimated the number of patients, the costs of medical insurance, and prognosis according to the treatment with or without endovascular thrombectomy (EVT) among in-patients with AIS.
Results
Since 2014, when EVT was covered by insurance, the number of patients who underwent EVT for AIS has increased significantly. Also, in the past decade, the medical costs following inpatient care for AIS with EVT have increased gradually, and the overall medical costs for the first year post-stroke have also increased. The prognosis of AIS patients with EVT was different according to the time of treatment. Annual trends for both mortality and cerebral hemorrhage after treatment of AIS with EVT have gradually decreased.
Ischemic stroke occurs when blood flow to the brain is interrupted due to narrowing or occlusion of a cerebral artery, causing irreversible brain damage if left untreated. Thus, early intervention is the key to a good prognosis [1,2]. In 2015, intracranial vessel thrombectomy was first recommended for patients with acute ischemic stroke (AIS) within 6 hours of stroke onset, and after 2 more clinical studies were published in 2018, the treatment coverage expanded to some patients with AIS up to 24 hours after stroke onset [1-3]. Since the use of tissue plasminogen activator (tPA) was approved in 1995, there have not been many improvements in clinical practice guidelines for patients with AIS until the advent of mechanical thrombectomy using a retrievable stent. The introduction of new treatment improved the prognosis and reduced mortality in patients with ischemic stroke [4-8]. On April 30, 2013, intracranial vessel thrombectomy using a retrievable stent was recognized as a new medical technology in Korea and was covered by insurance from August 1, 2014 [9].
To date, there has been no accurate report on the number of intracranial vessel thrombectomies performed annually in Korea. In 2016, the Korean Society of Interventional Neuroradiology (KSIN) conducted a survey in several hospitals performing endovascular thrombectomy (EVT) in Korea, and it is estimated that at least 2,300 procedures were performed that year [10]. Since 2015, after revising clinical practice guidelines covered by insurance, the number of procedures performed has increased significantly, which is consistent with the results of foreign studies [11]. The indications for intracranial vessel thrombectomy expanded in the 2018 American Stroke Association guidelines, and could also affect the 2019 KSIN guidelines [12], which may possibly increase the number of patients undergoing procedures in the future [13].
The purpose of this study was to evaluate trends in medical costs and prognosis in AIS patients in Korea from 2008 to 2017 using medical claims data and to analyze differences in medical costs and prognosis between patients treated before and after EVT as covered by healthcare reimbursement.
From National Health Insurance claims data, all medical claims of patients aged 45 or older admitted for an initial and principal diagnosis of ischemic stroke (Korean Standard Classification of Diseases, KCD: I63) between 2008 to 2017 were evaluated. The KCD code for thrombectomy was used to identify patients treated with EVT from the obtained database. On June 30, 2017, the revision of the Assessment Exception Criteria for Partial Co-payment resulted in a subdivision of the KCD code for thrombectomy. Thrombectomy was claimed as M6631 (thrombolysis-cerebral vessels) and M6633 (mechanical thrombectomy [catheter system]) before June 30, 2017; after that date, M6631 was subdivided into M6630 (thrombolysis-intracranial vessel) and M6635 (thrombolysis-extracranial cervical vessel), and M6633 into M6636 (mechanical thrombectomy-intracranial vessel) and M6637 (mechanical thrombectomy-extracranial cervical vessel). In addition, during the same period, patients who received tPA, an intravenous thrombolytic agent, were identified using product code 653500661 or Anatomic Therapeutic Chemical Classification System code B01AD02. Based on the extracted data, patients were classified into tPA, EVT, and EVT+tPA groups, respectively.
To evaluate treatment outcomes, death data was used as an outcome variable, and patients who died within 3 months and within 1 year after treatment were identified. Patients with ischemic stroke who have received thrombolytics or thrombectomy may undergo additional surgery due to adverse effects of treatment such as cerebral edema or hemorrhagic transformation secondary to ischemic stroke, and these patients are likely to have a poor prognosis. In order to identify patients who underwent surgery, patients with a principal diagnosis or first secondary diagnosis of cerebral hemorrhage (KCD: I61) or with procedure codes within 3 months after receiving a thrombolytic or thrombectomy were selected in the medical insurance claim. The extracted procedure codes were N0322 (Burr Hole), N0333 (craniectomy), S4756, and S4622 (craniotomy). To analyze medical expenditure, we checked the expenses per claim in every inpatient treatment for ischemic stroke and calculated the sum of all medical costs up to 1-year post-stroke.
We also classified patients based on tPA use and the period when EVT was performed. It was estimated that off-label stent retrievers were used in South Korea between October and December of 2010. Even though its usage was officially approved, stent retrievers were not reimbursed by the South Korean National Health Insurance between May 2013 and July 2014. Therefore, we categorized the period when stent retrievers were rarely used as the ŌĆ£non-advanced EVT period (January 2008 to December 2012)ŌĆØ, when we could not precisely identify stent retriever usage as the ŌĆ£transitional period (January 2011 to July 2014)ŌĆØ, and when the insurance claim data verified the frequency of stent retriever use as the ŌĆ£EVT period (August 2014 to December 2016).ŌĆØ
From 2008 to 2017, the number of patients treated with IV tPA tended to increase gradually. The number of patients receiving IV tPA treatment was 2,047 and 3,447 in 2008 and 2017, respectively, showing an increase of about 68.4% compared to 2008. In particular, the number of patients in 2014 increased by 25.7% compared to 2013, showing a significant increase compared to other time points. The number of patients who received EVT in 2008 and 2017 was 869 and 3,088, respectively, showing an increase of about 255% compared to 2008. There was a significant increase in patients who received EVT in 2015, 51.5% compared to the previous year. Since then, the number of patients has continued to increase until 2017 (Table 1).
In the tPA-only group, during the study period, the average inpatient cost per hospitalization was about 5,028,153 KRW (South Korean Won). From 2008 to 2015, this average inpatient cost remained at a similar level but has been increasing since 2016. Meanwhile, the cost for the EVT-only group averaged 11,205,949 KRW (┬▒6,462,243 KRW) per hospitalization. The average inpatient cost per hospitalization for the EVT-only group remained similar until 2013, but started to increase in 2014 and dramatically increased through 2016. For the total EVT group (EVT+tPA), the inpatient cost averaged 11,488,381 KRW (┬▒5,508,010 KRW) per hospitalization. Similar to the EVT-only group, the average inpatient cost per hospitalization showed an increasing trend from 2014 and has maintained an increase through 2017. The overall average medical cost was slightly higher than the EVT-only group (11,488,381 KRW vs. 11,205,949 KRW) (Fig. 1).
During the analysis period, the average 1-year cumulative medical cost after the onset of ischemic stroke in the tPA-only group was 18,569,845 KRW (┬▒19,382,107 KRW). The average 1-year cumulative medical cost for the tPA-only group have increased steadily every year. For the EVT-only group, 1-year cumulative medical cost after the onset of ischemic stroke averaged 28,466,009 KRW (┬▒23,168,003 KRW). Until 2013, there was no significant change in the average 1-year cumulative medical cost, but there was a tendency to increase significantly from 2014 to 2016. The average 1-year cumulative medical costs for the total EVT group (EVT+tPA) was 29,596,662 KRW (┬▒24,001,043 KRW). Similar to the EVT-only group, the average 1-year cumulative medical cost has tended to increase in 2014 and continued to increase sharply every year until 2016. Compared to the EVT-only group, the overall average 1-year cumulative medical cost for the total EVT group was higher, except in 2013 (Fig. 2).
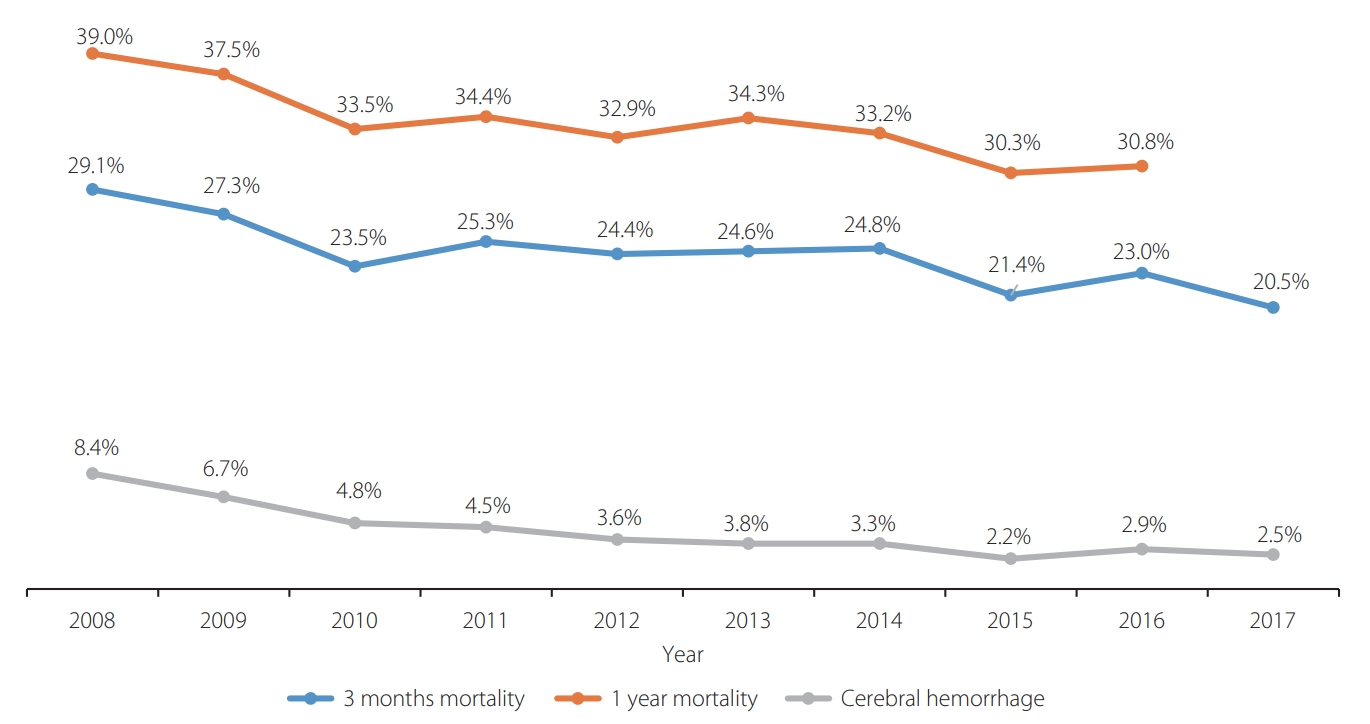
To evaluate the prognosis of patients with ischemic stroke, the number of deaths at 3 months and 1 year after undergoing IV-tPA treatment or EVT was determined. The 3-month mortality for the tPA-only group declined steadily from 2008 to 2017 (Fig. 3). Meanwhile, the 3-month mortality for the total EVT and EVT-only group declined more between 2009 and 2010 and 2014 and 2015 (Figs. 4, 5). The 1-year mortality for the tPA-only group also showed a tendency to decline gradually from 2008 to 2016, similar to the 3-month mortality. Likewise, the 1-year mortality for the total EVT and EVT-only group declined similarly to the 3-month mortality.
To analyze the prevalence of cerebral hemorrhage, we identified the percentage of patients whose surgical procedure codes for cerebral hemorrhage were claimed within 30 days after stroke onset. In the tPA-only group, procedure codes for cerebral hemorrhage were identified in 2.0% of patients within 30 days, and the rate decreased to 1.0% in 2017. Overall, the prevalence of cerebral hemorrhage declined from 2009 to 2013, then reached 1.3% (an increase of 0.15%) in 2014, but thereafter decreased again (Fig. 3). As a result of analyzing the total EVT and EVT-only group, the prevalence of cerebral hemorrhage within 30 days after ischemic stroke decreased from 6.8% (2008) to 2.1% (2017) in the total EVT group and 8.4% (2008) to 2.5% (2017) in EVT-only group (Figs. 4, 5).
Period-based trends revealed that the number of patients increased gradually during the study period (3,028, 4,113, and 5,360, respectively). The mortality rates decreased continuously from the non-advanced EVT period to the EVT period. Additionally, the ratio of patients receiving surgery for cerebral hemorrhage after EVT decreased during the study period (Table 2).
The AIS treatment strategy had a major turning point in 2015 with several randomized clinical trials (RCT) results [4-8], and EVT procedures in Korea have been expected to increase annually by about 30%. The reason for the increase in EVT procedures is thought to be the application of healthcare reimbursement for EVT since August 2014, along with the possibility of expanding treatment indications for EVT from the subsequent RCT [14,15]. This study showed that the number of patients treated with IV thrombolytics significantly increased in 2014, while the number of patients treated with EVT significantly increased in 2015.
The purpose of this study was to show annual trends in medical costs and the prognosis among patients who underwent recanalization treatment in AIS patients. In patients with AIS, the inpatient cost per hospitalization and 1-year cumulative medical costs after stroke onset gradually increased. It should be noted that the expanded scope of healthcare reimbursement for new medical devices, such as the retrievable stent, affects inpatient costs per hospitalization. In addition, it should be also noted that inpatient costs per hospitalization for patients with other types of ischemic stroke also show a steady upward curve [16].
Differences in the prognosis of patients with AIS who were treated with intravenous and/or intraarterial recanalization therapy were analyzed according to the time of treatment. Analysis of the annual trend showed that both the mortality and prevalence of cerebral hemorrhage gradually decreased in patients with AIS. In patients who underwent EVT, the 1-year mortality in 2016 decreased by about 10% compared to 2008. Considering the gradual increase in severity of patients with AIS due to an expanded time window, the introduction of new EVT seems to have a good effect on the prognosis of patients treated with AIS. Moreover, period-based analysis revealed that the patients treated with EVT had better outcomes in the EVT period than in the non-advanced EVT period.
The number of patients who need to be treated for AIS will inevitably increase in the future as the elderly population increases. According to the yearly trend, ischemic stroke accounted for 76% of all types of strokes in 2015 [17]. In order to reduce medical costs that are bound to increase in the future, it is necessary to establish an effective treatment system for patients with AIS. The inclusion of a new EVT in healthcare reimbursement has created an environment in which many hospitals can effectively treat patients with AIS. EVT can treat more AIS patients than IV tPA since it is used for up to 24 hours after the onset of symptoms in certain situations [14,15]. Although this study showed a gradual increase in medical costs in AIS patients, which may be in part because of the expanded scope in healthcare reimbursement for new medical devices such as the retrievable stent, it can be expected that the indirect socioeconomic costs could be reduced by improving the prognosis [18,19].
We could not verify the socioeconomic cost data from this claim data. Therefore, in a future study, there is a need to evaluate the relationship between EVT for AIS and changes in indirect socioeconomic costs as the basis for expanding the scope of healthcare reimbursement for AIS.
This study included several limitations. First, since this study analyzed medical claims data instead of actual hospital clinical data, so clinical factors that could affect the patientŌĆÖs prognosis were not determined. Also, there is a possibility that captured outcome events were not related to recanalization therapy but primary intracerebral hemorrhage, which was not associated with index ischemic stroke events. Second, it is difficult to determine the number of patients treated with a new EVT device, as the retrievable stent was still off-label or un-insured. Also, even after the retrievable stent was included in healthcare reimbursement, some patients were treated using different approaches such as suction catheters. So the possibility that these patients had some influence on the study results cannot be excluded. Third, considering the outcome, the most important outcome may be the modified Rankin Scale (mRS) and National Institute of Health Stroke Scale scores, which were not included in the healthcare data. Although the rate of cerebral hemorrhage may have decreased, the rate of disability (mRS of 3ŌĆō5 at 3-months) may have increased. The ratio of patients with an mRS of 3ŌĆō5 at 3-months could possibly affect the inpatient and 1-year cumulative medical costs, as some patients with an mRS of 3ŌĆō5 at 3 months can return to their daily lives after rehabilitation. So, when patients survive with a disability after a stroke event, their medical costs may increase. Lastly, in the case of patients with cerebral hemorrhage, only patients who had undergone surgical treatment could be included because brain imaging data were not obtainable. Therefore, it is highly probable that the prevalence of cerebral hemorrhage was measured as lower than the actual result since patients who died before arriving at the operating room or who did not require surgery were omitted from the study.
In this study, we showed that the number of patients who underwent EVT in AIS had significantly increased since 2014 and both inpatient medical costs and 1-year cumulative medical costs increased gradually. In addition, the prognosis progressively improved in patients who received EVT treatment among AIS patients. In a future study, there is a need to evaluate the relationship between EVT for AIS and changes in indirect socioeconomic costs as the basis for expanding the scope of healthcare reimbursement for AIS.
Notes
Fund
This study was supported by the Korean Society of Interventional Neuroradiology (KSIN) research grant 2019.
Ethics Statement
This study was approved by the Institutional Review Board of Ajou University Hospital. The consent for publication is not required as the submission does not include any images or information that may identify the person.
Fig.┬Ā1.
Change in inpatient cost per hospitalization for the tissue plasminogen activator (tPA)-only, endovascular treatment (EVT)-only, and total EVT groups. KRW, South Korean Won.
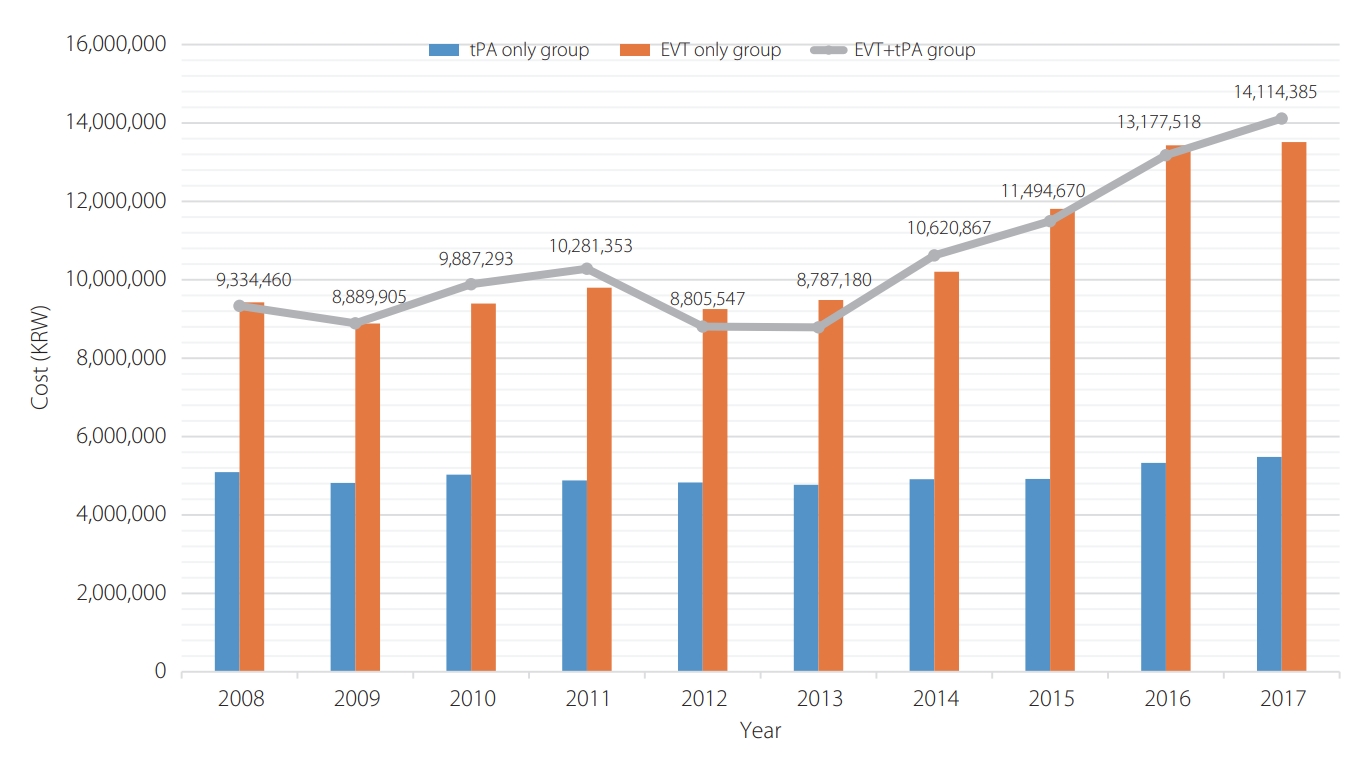
Fig.┬Ā2.
Change in the average 1-year cumulative medical costs for the tissue plasminogen activator (tPA)-only, endovascular treatment (EVT)-only, and total EVT groups. KRW, South Korean Won.
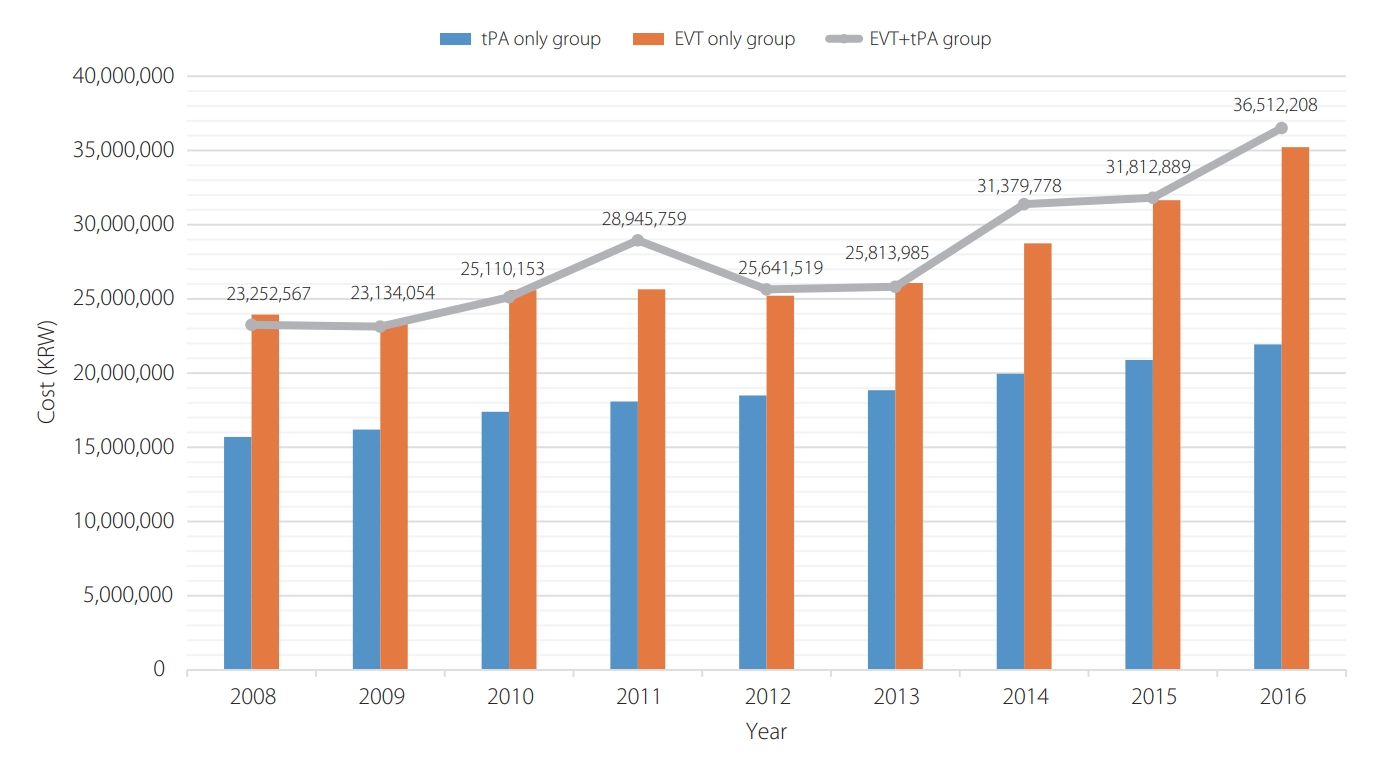
Fig.┬Ā3.
Time trends in 3-month, 1-year mortality, and cerebral hemorrhage for the tPA only group. tPA, tissue plasminogen activator.
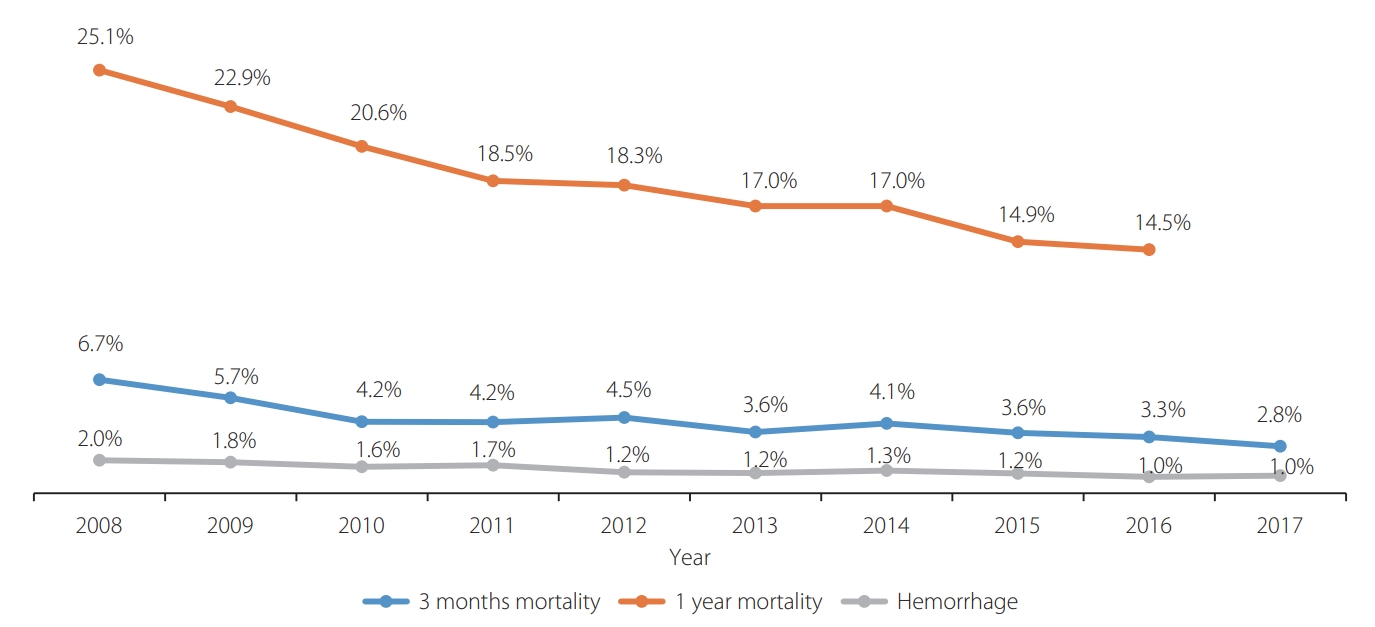
Fig.┬Ā4.
Time trends in 3-month, 1-year mortality, and cerebral hemorrhage for the total EVT group. EVT, endovascular treatment.
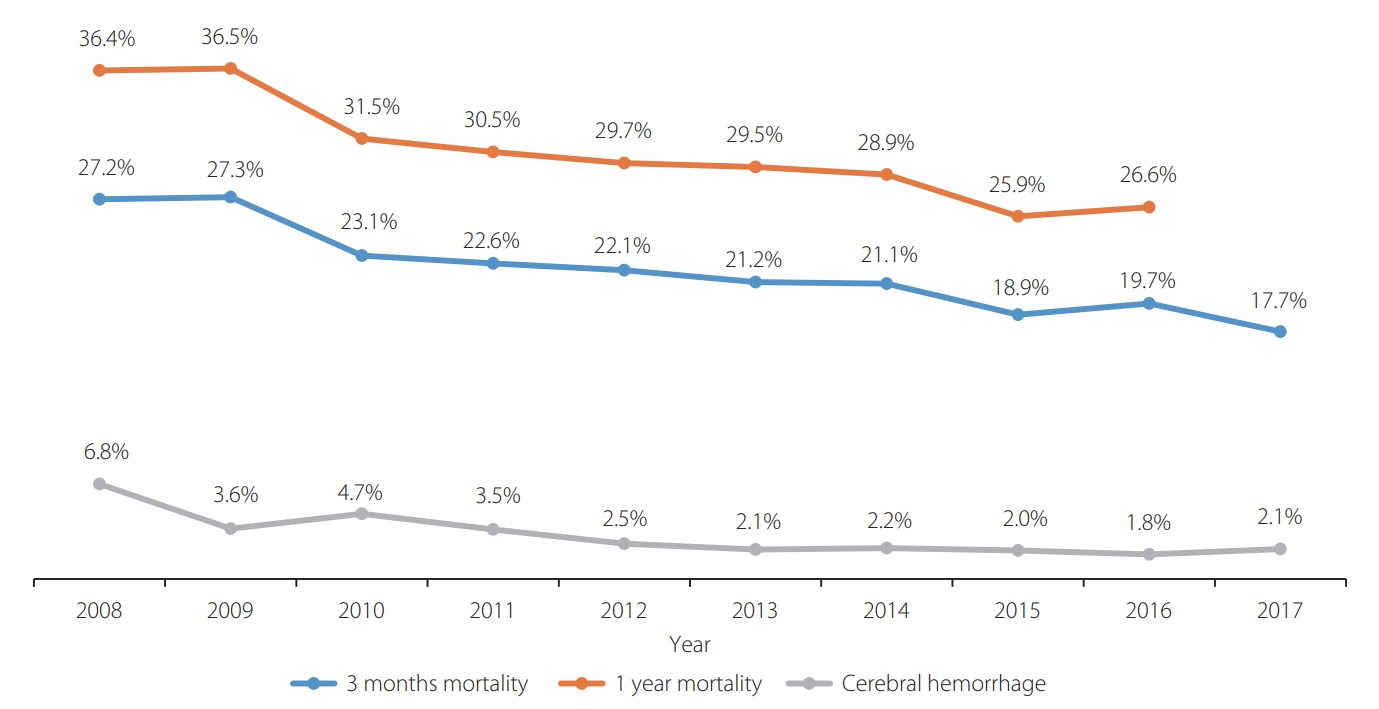
Fig.┬Ā5.
Time trends in 3-month, 1-year mortality, and cerebral hemorrhage for the EVT only group. EVT, endovascular treatment.
Table┬Ā1.
Yearly change in the number of patients undergoing intravenous tissue plasminogen activator (tPA) and endovascular treatment (EVT)
Table┬Ā2.
Period-based trends according to patient number and outcomes
REFERENCES
1. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al, American Heart Association Stroke Council. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:3020-3035.


2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al, American Heart Association Stroke Council. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018;49:e46-e110.


3. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581-1587.


4. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al, MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11-20.

5. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al, EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009-1018.


6. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al, ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019-1030.


7. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al, REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296-2306.


8. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al, SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285-2295.


9. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke 2016;18:102-113.




10. Seo KD, Suh SH. Endovascular treatment in acute ischemic stroke: a nationwide survey in Korea. Neurointervention 2018;13:84-89.




11. Furlan AJ. Stent-retriever thrombectomy for stroke. N Engl J Med 2015;373:1078
12. Ko SB, Park HK, Kim BM, Heo JH, Rha JH, Kwon SU, et al. 2019 Update of the Korean clinical practice guidelines of stroke for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke 2019;21:231-240.




13. Saber H, Navi BB, Grotta JC, Kamel H, Bambhroliya A, Vahidy FS, et al. Real-world treatment trends in endovascular stroke therapy. Stroke 2019;50:683-689.



14. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al, DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11-21.

15. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al, DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708-718.



16. Lim SJ, Kim HJ, Nam CM, Chang HS, Jang YH, Kim S, et al. Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database. J Prev Med Public Health 2009;42:251-260.


17. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke 2019;21:42-59.











