Depressed cranial fractures may complicate up to 6% of head injuries and account for significant morbidity and mortality [1]. Common complications from depressed skull fractures include infection, epilepsy, neurological deficits and mortality. Surgical treatment of compound depressed cranial fractures often involves debridement and elevation to decrease the incidence of infection. While not seen in teenagers or adults, a growing skull fracture is a rare complication of skull fractures in children usually less than three years of age. A hypothesized pathophysiological mechanism involves herniation of the leptomeninges with rupture of the dura during the skull fracture [2]. We encountered a rare case of intracranial hemorrhage secondary to a de novo distal middle cerebral artery (MCA) pseudoaneurysm within the exact location of an incompletely healed depressed skull fracture. The likely pathogenesis may have been the protrusion of brain parenchyma with associated vasculature through dural laceration sustained during initial brain injury and subsequent trauma from the incompletely healed bony defect between the skull and craniotomy. To our knowledge, there is no prior report of a traumatic pseudoaneurysm following a depressed skull fracture in the literature.
CASE REPORT
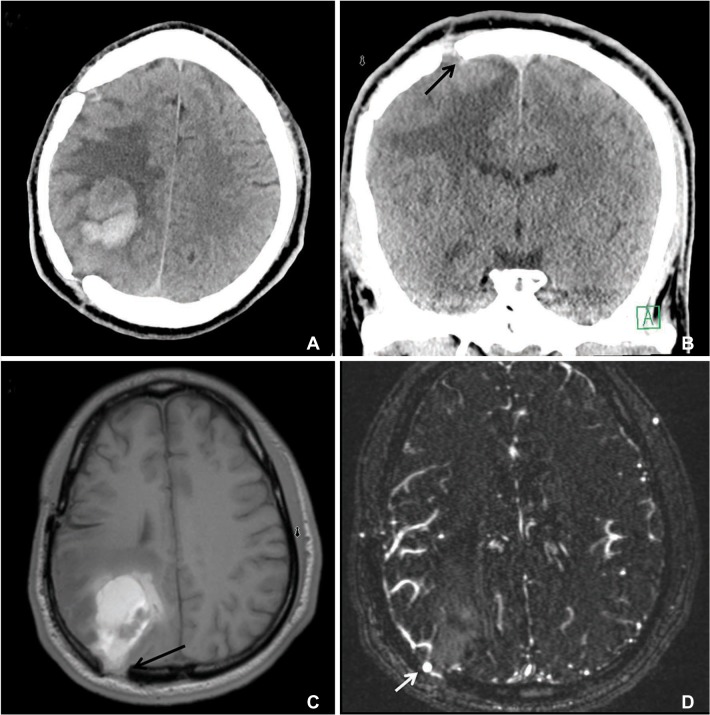
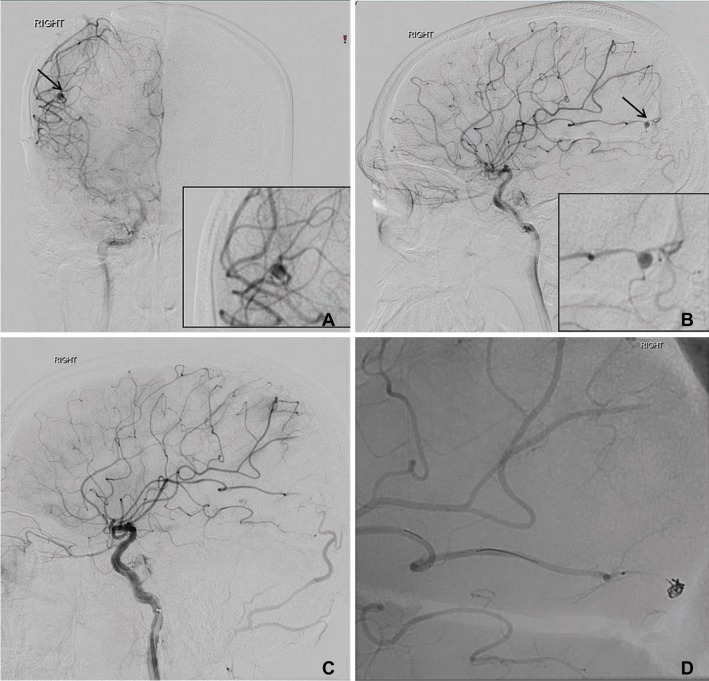
A 26-year-old male presented to us following a seizure with left sided weakness (4-/5, Medical Research Council (MRC) grade). The past medical history was significant for a traumatic brain injury seven years prior that involved a depressed skull fracture after being hit with a baseball bat. Craniotomy and repair of the depressed skull fracture occurred at an outside institution. A brain computed tomography (CT) scan at admission showed a 3.5 × 2.6 cm hematoma in the right parietal lobe adjacent to the prior craniotomy site. There was also bony separation at the margins of the prior craniotomy with presence of protrusion of the brain parenchyma through the defect (Fig. 1A, C). A magnetic resonance angiogram (MRA) of the brain suggested a pseudoaneurysm (Fig. 1D), which was confirmed on a catheter cerebral angiogram that demonstrated the presence of a pseudoaneurysm arising from the right middle cerebral artery M4 segment measuring 3 × 3 mm in size with a neck of 1mm that was successfully coiled (Fig. 2A, D). An excelsior SL-10 micro catheter (Stryker, Kalamazoo, Michigan, U.S.A.) was used for navigating the vascular anatomy, followed by deployment of a single platinum coil measuring 2.5 × 5 to achieve complete occlusion of the aneurysm. A new occlusion of the distal branches of the angular artery, likely thromboembolic, was identif ied on the f inal angiogram, but was regarded as clinically insignificant (Fig. 2C, D).
The post-operative course was uneventful with improvement in left-sided hemiparesis to almost normal strength, and the patient was discharged home on day three. He had been doing well at the 12-month follow-up, with no motor or sensory deficits and a modified Rankin scale score of 1. The patient does have occasional partial seizures likely from the prior depressed skull fractures (Engle class Ib), which are currently well-controlled with the use of medications.
DISCUSSION
Intracranial aneurysms can be classified as congenital, atherosclerotic, dissecting, infectious, and post traumatic [3]. Traumatic intracranial aneurysms (TICAs) are rare and account for less than 1% of the intracranial aneurysms and are more common in children and adolescents. They can occur after even mild or seemingly trivial head trauma, and are associated with a morbidity and mortality rate as high as 50%. The MCA has the most complex branching pattern of the major intracranial arteries and TICAs are frequently found in the cortical branches of middle cerebral artery (MCA) [4,5,6]. TICAs may develop beneath an overlying linear or depressed skull fracture and are attributed to direct vessel trauma leading to formation of a pseudoaneurysm.
Histologically, TICAs can be classified as true, false, dissecting or mixed based on the damaged structures of the vascular wall [4,5,7]. A pseudoaneurysm (false aneurysm), which is the most common type, occurs when all layers of the arterial wall are lacerated, and is almost always associated with direct injury to cortical arteries, which are often beneath a skull fracture. Several mechanisms have been proposed in the formation of traumatic aneurysms, all of which involve either direct injury to the vessel or stretching of the vessel by adjacent forces [6,8,9]. The case we encountered is very unusual, as the aneurysm did not develop from the direct trauma of the vessel from the depressed bone fragments; but rather occurred secondary to the outpouching of the brain parenchyma through the dural defect between the edges of the craniotomy flap and skull made during the initial repair of the depressed skull fracture (Fig. 1). This likely resulted in stretching and tearing of the arterial wall from the bony edges leading to formation of a pseudoaneurysm.
While debridement, elevation of the fracture, removal of bone fragments, and delayed cranioplasty (if needed) remains the most common way to manage depressed skull fractures, there is an increasing consensus that immediate bone fragment replacement/cranioplasty does not result in any increase in infectious complications and may be preferable as it also obviates the need for a second procedure [1,10]. Also, while prevention of infection and epilepsy remains the main driver of treatment for a compound depressed fracture, the present case highlights an unusual complication of a traumatic pseudoaneurysm formation that can be a cause of delayed morbidity and perhaps mortality. As the pseudoaneurysm likely resulted from the herniation of brain parenchyma through the dural defect, the likely pathogenesis involved presence of an occult dural tear that was sustained at the time of initial injury and was not apparent during the initial surgery.
CONCLUSION
A rare of case of a delayed traumatic pseudoaneurysm of the middle cerebral artery following surgical repair of a compound depressed fracture of the skull is reported. Being aware of this complication in providing long-term treatment to patients with depressed skull fractures can be helpful to avoid and treat this unusual complication.