Clinical Manifestation and Radiologic Patterns of Spontaneous Cervicocephalic Dissection According to the Anatomic Location: A Single-Center Analysis in Korean Patients
Article information
Abstract
Purpose
Spontaneous cervicocephalic dissection (SCAD) is an important cause of stroke and shows various lesion locations and clinical features. The purpose of this study was to analyze the location of SCAD and its clinical and radiologic patterns in Korean patients.
Materials and Methods
Patients with SCAD who were evaluated between 2013 and 2018 at a tertiary center in Korea were reviewed. We classified and compared the morphological (aneurysm or steno-occlusion) and presenting (hemorrhage or infarction) patterns according to the lesion locations (anterior circulation [AC] vs. posterior circulation [PC]; intradural [ID] vs. extradural [ED]).
Results
A total of 166 patients were included in this study. The SCAD most commonly occurred in the PC-ID location (65.1%), followed by AC-ID (13.3%), AC-ED (13.3%), and PC-ED (8.4%). Aneurysm and steno-occlusion patterns were observed in 66.9% and 57.8% of the cases, respectively. The aneurysm pattern was significantly more common in the PC-ID location (78.7%) than in other locations. As for the presenting pattern, cerebral infarction was the most common pattern (39.8%), and intracranial hemorrhage was observed only in the ID location (7.2%).
Conclusion
In Korean patients, PC-ID, especially ID vertebral artery, was the most common location of SCAD, and most cases were accompanied by an aneurysm. It also suggested that these location trends differ by population or ethnicity.
INTRODUCTION
Dissections are usually caused by an intimal tear, which allows blood to enter the artery wall and split its layers [1]. The result is either stenosis or aneurysmal dilatation of the vessel, depending on the location of the intramural hematoma within the vessel wall [2,3]. Spontaneous cervicocephalic dissection (SCAD) is an important cause of stroke, especially in young and middle-aged adults [4-7]. The incidence of spontaneous internal carotid artery dissection is approximately 2.5–3.0 per 100,000 individuals, and that of vertebral artery (VA) dissection is 1.0–1.5 per 100,000 individuals [1,8].
SCAD can be classified into anterior circulation (AC) (internal carotid artery [ICA], middle cerebral artery, and anterior cerebral artery) and posterior circulation (PC) (vertebrobasilar artery and posterior cerebral artery), and into intracranial and extracranial locations. Generally, the anterior and cervical (extracranial) arteries are the most commonly involved in Western countries [8-12], whereas the posterior and intracranial arteries are the most common dissection sites in Asians [2,7,13,14].
The various locations of dissections are related to their wide spectrum of clinical presentation. The two main presenting patterns of dissections are subarachnoid hemorrhage and cerebral ischemia [15]. It has been reported that subarachnoid hemorrhage, which can lead to devastating outcomes, represents 50–60% of the cases of intracranial dissection, and ischemic stroke or transient ischemic attack can be present in 30–78% [16]. However, in cases of cervical artery dissection, cerebral ischemia was reported in 67–90% of cases, and hemorrhagic presentations were rare [9,12,17].
In previous studies, the common location and clinical aspects of dissections significantly varied [2,9-14,17], which is likely due to differences in ethnicity and study design. Therefore, we analyzed the presenting pattern and lesion morphology according to the lesion site in consecutive patients with SCAD who were evaluated at a large tertiary hospital in Korea and compared the results with previous studies performed in other countries.
MATERIALS AND METHODS
Patients and Clinical Characteristics
The Institutional Review Board of our center approved this study (No. 2021-0778) and waived the need for written informed consent considering its retrospective design. This study included consecutive patients with SCAD from the prospectively collected database of our tertiary referral center between 2013 and 2018. The diagnosis of SCAD was made if any typical signs of dissection (double lumen, intimal flap, intramural hematoma, or pseudoaneurysm) were identified on various imaging modalities. Digital subtraction angiography (DSA) was performed in all patients (n=166). Additionally, we reviewed the results of other imaging modalities for confirmation of the diagnosis and morphological pattern analysis, including vessel wall magnetic resonance imaging (MRI) (n=100), magnetic resonance angiography (MRA) (n=150), computed tomography angiography (CTA) (n=87). We excluded cases with vascular abnormalities of uncertain etiology, dissections secondary to surgical or interventional procedures, major trauma, moyamoya disease, or vascular malformations. The process of patient selection and the results of pattern analysis are summarized in Fig. 1.

Flow chart of the dissection analysis and comparison with other studies. CTA, computed tomography angiography; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; DSA, digital subtraction angiography; AC, anterior circulation; PC, posterior circulation; ID, intradural; ED extradural. *Number of patients undergoing each modality.
Risk factors for SCAD, including massage, manipulation, minor trauma, exercise, and hypertension, were retrieved from the database. Clinical manifestations were categorized based on the chief complaint at the time of symptom onset and visit to the hospital.
Lesion Locations
The lesion locations were identified and differentiated between AC vs. PC and intradural (ID) vs. extradural (ED) location, and were thus divided into four groups as follows: (1) AC-ID, (2) AC-ED, (3) PC-ID, and (4) PC-ED. Considering the potential risk of subarachnoid hemorrhage in ID lesions, the cervicocephalic arteries were divided into ID and ED.
AC was defined as the vascular territories of the ICA, excluding the posterior communicating artery. PC was defined as the vascular territories of the vertebrobasilar artery, including the posterior communicating artery. Thus, the dura mater was used as the anatomical boundary between ID and ED. The origin of the ophthalmic artery from the ICA was regarded as the surrogate for the location of the dura mater for AC [18]. For PC, the point at which the VA passes through the dura mater to reach the subarachnoid space was regarded as the boundary between ID and ED.
Analysis of Morphological and Presenting Patterns
For pattern analysis, findings of DSA, MRA, and CTA were reviewed by two interventional neuroradiologists and an interventional neurologist (more than two years of experience in neurovascular imaging). The lesions were categorized into three morphological patterns depending on the angiographic imaging findings: (1) aneurysm (luminal ectasia in the dissected segments larger than the diameter of the normal segment), (2) luminal stenosis or occlusion of the lumen compared with the adjacent normal segment, and (3) combined (both aneurysmal dilatation and stenosis). Patients were also classified into three groups according to the presenting pattern: (1) intracranial hemorrhage, (2) cerebral infarction, and (3) none.
Comparison for the Ethnic Difference Using Data from Previous Studies
We compared our data with those of studies from different ethnic populations in order to overcome the limitation of the lack of a control group considering the rarity of the disease as well as possible ethnic differences in lesion characteristics. We searched for studies that included (1) more than 100 patients from an Asian country or a Western country, (2) both intracranial and neck locations, and (3) diagnosis of dissections by vessel wall MRI or DSA. Accordingly, we selected the study by Tsukahara and Minematsu [14] for comparison with another Asian country (Japan), and the study by von Babo et al. [19] for comparison with European countries (France and Switzerland). Of the many studies performed in Asian countries that satisfied the search criteria, the multicenter study by Tsukahara and Minematsu [14] had the largest number of study patients (n=454). Other studies on SCAD that were not included in the comparison are also discussed in the Discussion section.
Statistical Analysis
Continuous variables are expressed as means and ranges, and categorical variables are expressed as frequencies with percentages. Fisher’s exact test was initially used for the comparison of sex, risk factors, clinical manifestation, and morphological and presenting patterns according to the lesion locations. Then, if a statistically significant difference was observed among the four anatomic locations, pairwise Fisher’s exact test was used to evaluate which combinations of sites had significant differences. Presenting patterns were compared among the three morphological patterns of dissection using Fisher’s exact test and pairwise Fisher’s test. To compare our data with those of two previous studies, presenting patterns and locations of dissections were compared in the same stepwise manner as described above. Statistical analysis was conducted using the SPSS Statistics version 21 (IBM Co., Armonk, NY, USA) and R (R Foundation for Statistical Computing, Vienna, Austria). P-values smaller than 0.05 were considered statistically significant.
RESULTS
Patients and Clinical Characteristics
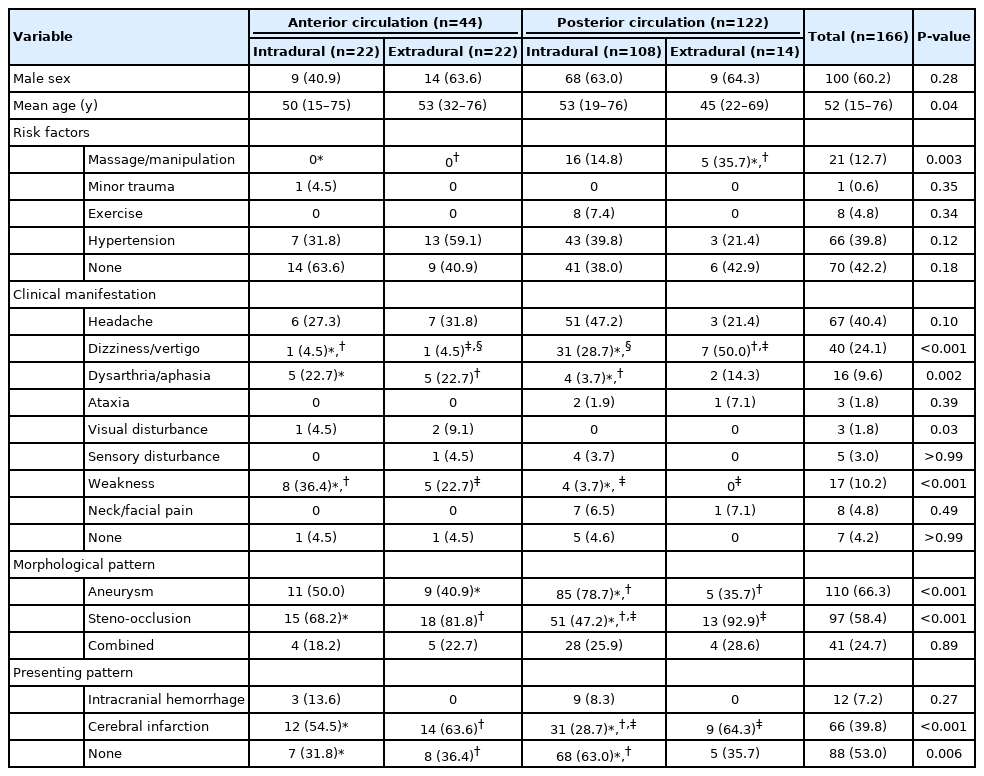
A total of 166 patients (mean age, 52 years; 100 [60.2%] men) were included in this study. The clinical characteristics and dissection patterns according to the lesion location are shown in Table 1. The distribution of ID and ED locations was significantly different between AC and PC lesions (P<0.001). Among those with PC lesions (n=122), ID location was dominant (n=108; 88.5%); among those with AC lesions (n=44), ID (n=22) and ED locations (n=22) were equally distributed. Among those with ID lesions (n=130), PC was more common (n=108; 83.1%); among those with ED lesions (n=36), AC was more common (n=22; 61.1%).
History of massage or manipulation of the neck was only present in those with PC dissection, and more common in PC-ED than in PC-ID (35.7% vs. 14.8%, P=0.09). The proportions of patients with minor trauma, exercise, and hypertension were not significantly different according to lesion location. While dizziness/vertigo was significantly more common in PC than in AC (31.1% vs. 4.5%; P<0.001), there was no significant difference between PC-ID and PC-ED (28.7% vs. 50.0%, P=0.15). Dysarthria/aphasia was more common in AC-ID (22.7%) and AC-ED (22.7%) than in PC-ID (3.7%) (P=0.02). While weakness was observed in 29.5% of cases with AC, it was rarely observed in PC (3.7%), all of which were found in cases with PC-ID. Visual disturbances were only reported in AC (6.8%).
Morphological and Presenting Patterns According to Lesion Location
Morphological patterns were significantly different according to the lesion location (P<0.001) (Table 1). Aneurysm, steno-occlusion, and combined patterns were observed in 110 (66.3%), 66 (39.8%), and 41 (24.7%) patients, respectively. The aneurysm pattern was observed predominantly in PC-ID (78.7%) over ED locations. On the other hand, the proportion of the steno-occlusion pattern in the PC-ID location (47.2%) was significantly smaller than that in other groups (68.2–92.9%).
The distributions of presenting patterns according to the lesion location are shown in Table 1. Intracranial hemorrhage only occurred in ID dissections, and there was no significant difference between the AC (13.6%) and PC (8.3%) groups (P=0.27). In contrast, cerebral infarction was significantly less common in PC-ID (28.7%) than in other locations (54.5–64.3%) (P<0.001), in which cerebral infarction was the most common presenting pattern.
The presenting pattern was significantly different according to the morphology of the dissection (Table 2). Intracranial hemorrhage exclusively occurred in the aneurysm pattern (17.4%). In contrast, cerebral infarction was observed in all patterns, but significantly more in the steno-occlusion (67.9%) and the combined (53.7%) patterns (P<0.001).
Comparison with Other Ethnic Populations
Table 3 shows the comparison between the results of the current study and those of two previous studies from European countries (France and Switzerland) and Japan that included 970 (mean age, 45 years; 579 [59.7%] men) and 454 (median age, 54 years; 318 [70.0%] men) patients, respectively [14,19]. Male predominance was significantly higher in the Japanese study than in other studies.
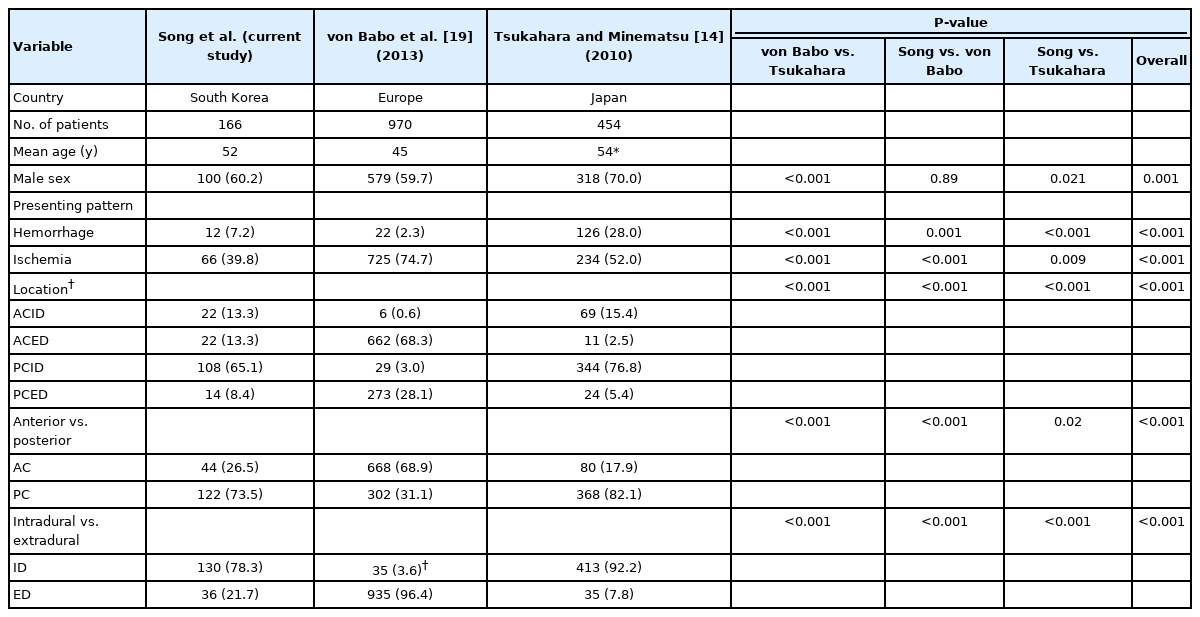
Comparison of studies reporting presenting pattern and location of intracranial and cervical artery dissection
Regarding the SCAD location (Fig. 2), PC was more common in the Japanese study compared with the current study (82.1% vs. 73.5%, P<0.02). Conversely, in the European study, the involvement of PC in the SCAD (31.1%) was significantly lower than in the Korean and Japanese studies. Among PC dissections, ID location was predominant in the current study (88.5%) and the Japanese study (93.5%), while the prevalence of ID location was significantly lower in the European study (9.6%; P<0.001). Among AC dissections, ID locations (86.3%) were more common in the Japanese study, whereas ED locations (99.1%) were predominant in the European study. In this Korean study, ID and ED were evenly observed in the AC dissections.
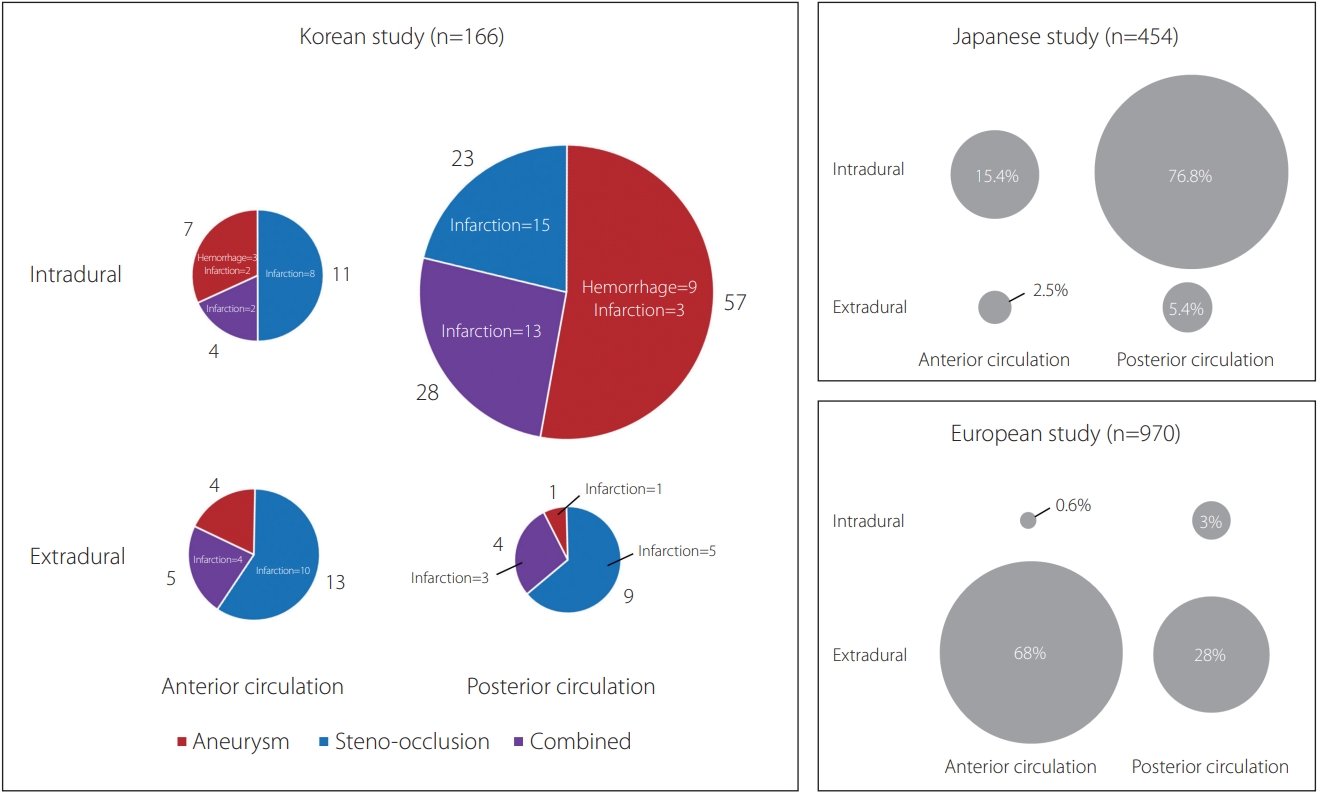
Pie charts showing the differences of lesion locations among three studies according to the presenting and morphological patterns. The sizes of the circles reflect the number of patients in each group. The sector of the circle is marked with different colors according to the proportional patient number of each morphological pattern; the numbers of “aneurysm” and “steno-occlusion” do not include the numbers of “combined” cases. The pie charts of Japanese and European studies do not have colors because a detailed analysis of presenting patterns could not be done.
The presenting pattern of dissection was significantly different among the three studies (Table 3). The incidence of intracranial hemorrhage in this study (7.2%) was lower than that of the Japanese study (28.0%, P<0.001) but higher than that of the European study (2.3%, P=0.001). The prevalence of ischemia (cerebral infarction and transient ischemic attack) in this study (39.8%) was significantly lower than those in the European (74.7%) and Japanese (52.0%) studies.
DISCUSSION
In this study of Korean patients with SCAD, intradural VA dissection with an aneurysm was the most common presenting pattern. Dissection was more commonly observed in the PC (73.5%), in which ID location was the majority (88.5%). Aneurysms were the most predominant morphological pattern (78.7%) in PC-ID dissections, whereas steno-occlusion was more common in other locations. In terms of lesion location, the results of our current study and a Japanese study were significantly different from that of a European study, in which most of the PC dissections were in the ED location.
In our study, dissection involving PC accounted for 73.5% of the SCAD. Several East Asian studies, in which intracranial dissection was dominant (65.9–92.2%), reported that 60% to 82% of dissections were in the PC, which is similar to our results [2,3,7,13,14,20,21]. In contrast, previous studies in North America and Europe, which exclusively consisted of cervical (extradural) dissections, reported that the AC (63–69%) was more commonly involved [9,10,12,17].
The ratio of AC and PC was shown to be different between ID and ED lesions in previous studies. In several sizable studies on intracranial artery dissection in Japan, Korea, and Finland [16], intracranial dissections affected the PC more frequently (75–93%). Similarly, in the only large study in the West that included intracranial dissection in both AC and PC, majority (82.8%) of intracranial dissection occurred in the posterior circulation [19]. In the contrary, cervical artery dissections involve the AC more (62–71%) in most studies, including Western and Eastern [2,9,10,12,13,17,19]. The fundamental reason for the higher prevalence of PC dissections in East Asia and AC in Western populations is possibly that intracranial lesions, which occur mainly in PC, predominate in East Asia and are rare in the West.
It is unknown why the rate of intracranial artery dissection is higher in Asians than in Westerners. This may be related to the fact that intracranial atherosclerotic disease and moyamoya disease are also more prevalent in Asians than in Western populations; the reason for this is also unknown [22-25]. The predominance of intracranial artery dissection in certain ethnic groups or children suggests that there may be genetic susceptibilities contributing to the intracranial artery dissection [4,16,26]. It has been reported that SCAD may be a complication of monogenic connective tissue diseases, such as vascular Ehlers-Danlos syndrome [27] and Marfan syndrome [28]. In addition, some studies have shown that variations in genes such as ICAM-1 [29] (intercellular adhesion molecule 1), RNF213 (ring finger protein 213) [30], and MTHFR [31] (methylenetetrahydrofolate reductase) may be associated with SCAD. Also, one report showed that cervical arterial tortuosity is related to dissection [32], which suggests that genetic diseases showing congenital vascular weakness such as arterial tortuosity syndrome may also play a role in SCAD.
In our results, aneurysms were more common in ID dissections (73.8%) than in ED dissections (38.9%), and most commonly observed in PC-ID (78.7%). Compared with the cervical artery, the intracranial artery relatively lacks elastic fibers in the media and adventitial tissue and has no external elastic layer [8,33]. Therefore, intracranial dissection is more likely to develop dissecting aneurysms due to the lack of supporting tissue in the vessel [34]. The reason why aneurysms are more commonly found in the posterior circulation in the intradural dissection is still unclear.
History of minor trauma, massage, or manipulation of the neck was more common in PC-ED (35.7%) than in PC-ID (14.8%), which is similar to the results of other studies that examined the differences between intracranial and extracranial VA dissections [21,35]. Hypertension and old age were observed more frequently in PC-ID than in PC-ED, supporting findings from previous papers that suggested that atherogenic factors influence intracranial VA dissection [21].
There are several limitations to this study. First, this study was performed at a single tertiary referral center and only included patients who underwent DSA, which may have led to a selection bias that favored the inclusion of patients with more severe dissection. In addition, the results of this data were obtained from a single center and cannot be representative of Korea, therefore, comparison with multicenter studies in Japan and Europe may be limited. Second, prognostic factors and outcomes after treatment were not elucidated in this study. Further studies are needed to identify those who might benefit from endovascular treatment and those who may be sufficiently managed using conservative treatment. Third, considering the dynamic nature of dissections, it would have been better if the period between the onset time and the imaging time was analyzed; however, the retrospective design of the study did not allow for the estimation of the exact time of occurrence.
CONCLUSION
In conclusion, our study showed that PC-ID, especially intradural VA, was the most common location of SCADs in Korean patients, which is similar to the results of a Japanese study and different from those of a European study. SCADs showed diverse presenting and morphological patterns according to the lesion location, as cerebral infarction was the most common presenting pattern in all locations, while hemorrhage was observed only in ID dissection. Aneurysm was the most common morphological pattern of PC-ID, and steno-occlusion was the most common finding in AC and PC-ED.
Acknowledgements
We thank Minkyu Han, PhD for his help in statistical analysis. We also acknowledge Prof. Hee-Joon Bae in Seoul National University Bundang Hospital for his help in comparing our data with those of previous studies.
Notes
Fund
The study was sponsored by a grant from the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2018R1A2B6003143).
Ethics Statement
The Institutional Review Board (IRB) of our center approved this study (No. 2021-0778). The IRB waived the need for written informed consent considering its retrospective design. The Consent for publication is not required as the submission does not include any images or information that may identify the person.
Conflicts of Interest
DCS has been the Editor-in-Chief of the Neurointervention since 2018. No potential conflict of interest relevant to this article was reported. YS has been the Assistant Editor of the Neurointervention since 2019. No potential conflict of interest relevant to this article was reported. No other authors have any conflict of interest to disclose.
Author Contributions
Concept and design: DCS. Analysis and interpretation: YS, SIP, PB, and BK. Data collection: SIP, PB, and BK. Writing the article: YS and SIP. Critical revision of the article: DCS and YS. Final approval of the article: DCS, YS, SIP, PB, and BK. Statistical analysis: SIP. Obtained funding: DCS. Overall responsibility: DCS.