Fracture of a Flow Diverter in the Cervical Internal Carotid Artery Due to Eagle Syndrome
Article information
Abstract
In Eagle syndrome, elongated styloid processes may provoke internal carotid dissection and pseudoaneurysm causing stroke and data regarding possible complications or long-term results of pseudoaneurysm treatment using a flow diverter are limited. We report a case of a dissection-related pseudoaneurysm in the left cervical carotid artery treated by implantation of a flow diverter. Follow-up imaging of the flow diverter showed fracture of a continuous radiopaque marker at 3 months and fracture of a second continuous radiopaque marker at 7 months, while contrasting of the vessel was preserved. At the time of angiographic control (8 months after implantation), the flow diverter and the extracranial left internal carotid artery were occluded, and the patient did not experience any symptoms throughout the period.
INTRODUCTION
In Eagle syndrome, an elongated styloid process or calcified stylohyoid ligament may cause intermittent dysphagia, foreign body sensation, and pain in the neck, throat, or face [1]. Additionally, this elongated styloid process can also result in vascular injury, usually dissection of the internal carotid artery (ICA), due to its anatomical proximity to the vessel, possibly leading to the formation of a pseudoaneurysm [2].
There are several options to treat the symptoms of Eagle syndrome, such as medical or surgical management, but there is no broad consensus. Implanting a flow diverter to treat cervical pseudoaneurysms is a possible treatment option [3-6]. Due to the small number of reported cases, experience and knowledge of possible complications is limited.
CASE REPORT
History and Examination
After physical exercise, a patient in their 40s presented with ptosis and flickering visual disturbance in the left eye and was admitted to our hospital for a minor stroke (National Institutes of Health stroke scale, 1; modified Rankin scale, 1) due to a dissection of the left ICA, which was likely due to an elongated styloid process of 5.4 cm length (Fig. 1A). Seven days later, the patient experienced transient numbness in the right hand. Due to these mild neurological symptoms, the patient was heparinized and discharged home without any symptoms or disabilities.
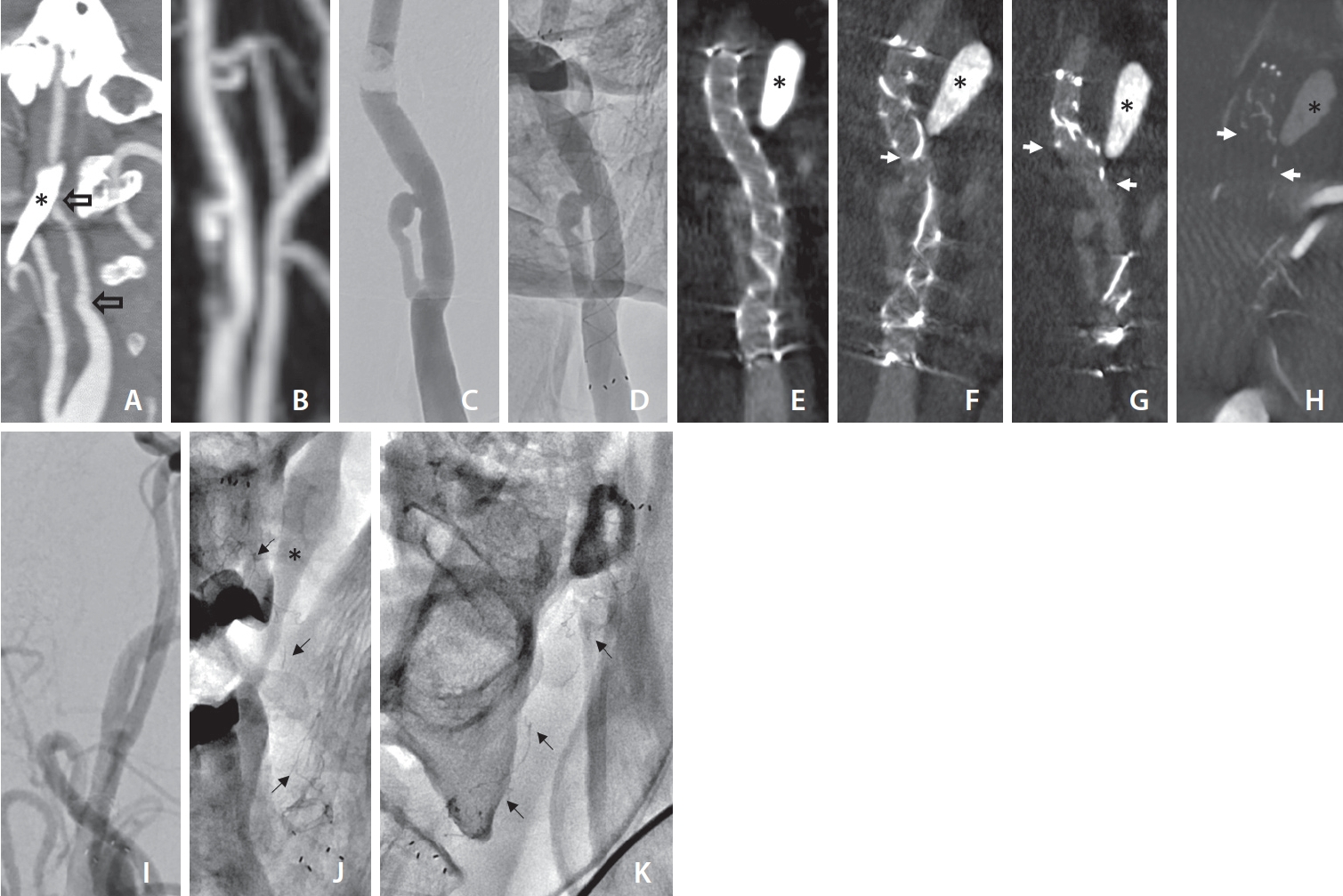
Sagittal images of computed tomography (CT) angiography at first presentation of a patient with minor stroke showing the elongated styloid process (asterisk) and a caliber reduction of the left internal carotid artery (ICA) secondary to dissection. (A) The blank arrows indicate the proximal and distal entry of the dissection, later to become the pseudoaneurysm. (B) Contrast-enhanced magnetic resonance angiography (posteroanterior [PA] view) of the left ICA showing a pseudoaneurysm after 6 months. Digital subtraction angiography (DSA) image of the left carotid artery pseudoaneurysm before (C) and corresponding non-subtracted angiography image after (D) implantation of the flow diverter. Coronal multiplanar reconstruction of flat-panel CT with intravenous contrast: on day 1 (E), at 3 months (F), and at 7 months (G) after flow diverter implantation. Note: despite the implanted flow diverter, the pseudoaneurysm still fills with contrast agent (E–G). (H) Coronal multiplanar reconstruction of flat-panel CT after intra-arterial contrast medium injection in the left ICA at 8 months after implantation. The white arrows on the follow-up images indicate the fractured and retracted distal radiopaque struts of the flow diverter. (I) DSA image (PA view) of the flow diverter 8 months after implantation showing occlusion of the device and the ICA. Single shot X-ray of the fractured flow diverter in PA (J) and lateral view (K). The black arrows point to fragments of the radiopaque struts of the flow diverter.
Follow-up magnetic resonance imaging 6 months after the index event showed the formation of a pseudoaneurysm of the left ICA (Fig. 1B). Due to a risk of thrombus formation within the pseudoaneurysm, the patient was started on dual platelet inhibition (acetylsalicylic acid 100 mg once daily and Clopidogrel 75 mg once daily) and scheduled for endovascular treatment.
Treatment
Selective cervical angiography was performed with a straight 6 Fr/100 cm guiding catheter (Asahi Fubuki; Asahi Intecc CO., Ltd.) by a transfemoral approach, via an arterial sheath, under general anesthesia. Angiography of the left ICA demonstrated a double lumen forming a pseudoaneurysm with an undulating vascular caliber and a total length to reentry into the true lumen of 13 mm (Fig. 1C). A microcatheter (0.027 Headway; MicroVention) was used to position and implant a 5.5 mm×32/26 mm dual-layer flow-diverting stent (Flow Re-Direction Endoluminal Device; MicroVention Inc.) covering both the entrance and the exit of the pseudoaneurysm (Fig. 1D). After deployment, the proximal and distal widths of the flow diverter were 5.3 mm and 3.8 mm, respectively.
Outcome and Follow-up
Control imaging on the first postoperative day using flat-panel computer tomography with intravenous contrast medium administration showed an intact flow diverter with good wall apposition and continuous contrast flow of the left ICA (Fig. 1E). The patient was discharged home and presented for follow-up examinations 3 and 7 months after the treatment without having experienced any symptoms in the meantime. Follow-up imaging of the flow diverter showed fracture of a continuous radiopaque marker at 3 months and additional fracture of a second continuous radiopaque marker at 7 months (Fig. 1F, G). The inner micromesh of the flow diverter could not be assessed on the scheduled imaging. However, in follow-up imaging, the contrast agent in the left ICA, the pseudoaneurysm, and the flow diverter could be visualized without any change. During angiographic control 8 months after implantation, the flow diverter and the extracranial left ICA were occluded without causing symptoms (Fig. 1H–K).
DISCUSSION
In adults, the styloid process is approximately 2.5-cm–long, and its tip is located between the external and internal carotid arteries, just lateral to the tonsillar fossa. It may develop inflammatory changes or impinge on adjacent arteries or sensory nerve endings, leading to the symptoms described as Eagle syndrome. The treatment of Eagle syndrome is primarily surgical. The styloid process can be shortened through an intraoral or external approach.
Possible complications of Eagle syndrome, i.e., the dissection of the ICA, are treated with either medication, surgery, or endovascularly, depending on the clinical symptoms and risk for further complications, such as an ischemic stroke. A surgical therapy option for a pseudoaneurysm, possibly in combination with resection of the styloid process would be an open vascular surgical procedure [7-9]. Another option for treating a pseudoaneurysm in the cervical ICA is endovascular treatment using carotid artery stenting, possibly using a covered stent or a flow diverter. With flow diverters, satisfactory angiographic and clinical results have been achieved in treating carotid artery pseudoaneurysms in a small number of cases [3-6]. The disadvantage of endovascular therapy may be from the residual styloid process. Due to the small number of cases, experience, and knowledge of possible complications after the implantation of flow diverters for the treatment of pseudoaneurysms, especially in the case of Eagle syndrome, is limited. Any stent, conventional or covered stent, would need to withstand the forces of the elongated styloid process and would therefore also run a risk of fracture analogous to the flow diverter in this case report.
Our case is, to our knowledge, the first reported case of delayed stent fracture of a flow diverter to treat a cervical artery pseudoaneurysm due to the adjacent elongated styloid process. There are isolated case reports describing a fracture or compression of a stent in the ICA [10,11]. However, these patients were treated using conventional carotid stents for an ischemic stroke due to arterial dissection. Since flow diverters are more flexible than conventional carotid stents due to their material properties, it has been assumed that they are better tolerated with a lower risk of complications in the treatment of cervical pseudoaneurysms. Our case shows that not only the vessel but also vascular implants, such as flow diverters, can be damaged by an elongated styloid process and cause occlusion of the ICA. Following the permanent insertion of a flow diverter, covered stent, or conventional stent, material wear, fatigue, or breakage might occur, even after several months or years, due to stress in the movable segment of the neck. Duarte–Celada and colleagues report a case in which elective styloidectomies of the right and then left styloid processes at 5 and 8 months, respectively, were performed after stent placement in a patient with Eagle syndrome initially presenting with bilateral carotid dissection [12]. It remains unclear whether the subsequent removal of the styloid processes was carried out to protect the implanted covered stents or to reduce other symptoms caused by the styloid processes, such as headaches and neck pain. However, the 2-year follow-up computed tomography angiography demonstrated bilateral stent patency.
In summary, it remains important to convey that elongated styloid processes cannot only induce vascular injury but can also damage implanted flow diverters leading to vascular occlusion. Surgeons must be aware of this risk and carefully weigh treatment alternatives and the choice of material.
Notes
Fund
None.
Ethics Statement
The Institutional Review Board waived the need for a seperate ethics approval since this is a retrospective case report. The patient provided written informed consent for the publication of the case report.
Conflicts of Interest
The authors have no conflicts to disclose.
Author Contributions
Concept and design: JARP. Analysis and interpretation: JARP. Data collection: JARP. Writing the article: JARP and FW. Critical revision of the article: JARP, FW, and MK-O. Final approval of the article: JARP, FW, and MK-O. Overall responsibility: JARP.
