Facilitated Retrograde Access via the Facial Vein for Transvenous Embolization of the Cavernous Sinus Dural Arteriovenous Fistula with Isolated Ophthalmic Venous Drainage
Article information
Abstract
Management of cavernous sinus dural arteriovenous fistula (CSDAVF) continues to present significant challenges, particularly when the inferior petrosal sinus is thrombosed, collapsed, or angiographically invisible. In this study, we introduce facilitated retrograde access via the facial vein, which is employed in the transvenous embolization of CSDAVF with isolated superior ophthalmic venous drainage. We also present illustrative cases and technical points.
INTRODUCTION
Cavernous sinus dural arteriovenous fistula (CSDAVF) is described as an abnormal arteriovenous connection that involves the dura mater within or adjacent to the walls of the cavernous sinus (CS) [1]. Transvenous embolization via the inferior petrosal sinus (IPS) remains the most preferred venous route for accessing the shunt hole. Nonetheless, this route may become thrombosed, collapsed, or angiographically invisible on occasion [2]. Although alternative venous routes have been investigated, including the superior petrosal sinus and facial vein, the IPS, whether ipsilateral or contralateral to the shunt hole, remains as the primary venous access route to the CS [1-4].
In the case of CSDAVF characterized by isolated venous drainage via the ophthalmic vein, direct access to the ophthalmic vein is suggested to be a viable approach to the shunt hole [5,6]. However, this approach is not preferred at our institution as it necessitates surgical exposure of the ophthalmic vein before direct access can be achieved and requires manipulation of neurointerventional devices over the patient’s neck.
Several difficulties are encountered in achieving retrograde endovascular venous access to the superior ophthalmic vein, including complex and lengthy retrograde routes from the superior vena cava to the superior ophthalmic vein, potential anatomical variation in internal or external jugular vein tributaries, and tortuosity at the junction among the superior ophthalmic supraorbital and angular veins [6].
In this study, we present a feasible method that facilitates retrograde venous access to the ophthalmic vein via the facial vein in patients with CSDAVF who exhibit isolated ophthalmic venous drainage.
CASE REPORT
Case 1
A patient in their early 60s presented with sudden bilateral proptosis and conjunctival injection. Subsequent magnetic resonance imaging (MRI) suggested the possibility of a CSDAVF. The diagnosis was confirmed by digital subtraction angiography (Fig. 1A), which showed a shunt hole at the superior posterior region of the predominantly atretic right CS. The feeding vessels were identified as dural branches of the ipsilateral internal carotid artery. Contrarily, the left CS generally preserved its channel-like architecture. The 2 sinuses were interconnected via a dilated intercavernous sinus. The venous drainage had divergent routes specifically through the right and left superior ophthalmic veins. The left superior ophthalmic vein exhibited greater dilation than its right counterpart. Other venous pathways, such as the petrosal sinus or cortical veins, were absent. No improvements were observed in the symptoms and imaging findings after conservative management and throughout the 6-month follow-up. Consequently, endovascular treatment was administered to treat the fistula. Fistula access via the superior ophthalmic veins was selected due to the considerable distance between the residual sac and the ipsilateral proximal opening of the IPS. Under general anesthesia and systemic heparinization, a 4-French diagnostic catheter (Jungsung Medical) was inserted into the right internal carotid artery through the left femoral artery for control angiography and then a 6-French long sheath (Shuttle; COOK Medical) into the left brachiocephalic vein through the right femoral vein. The long sheath was further advanced into the left external jugular vein with navigational assistance from a roadmap acquired by the diagnostic catheter. While the tip of the long sheath was positioned downstream in the left external jugular vein, the microcatheter (Prowler 10; Cerenovus) and microwire (Traxcess; MicroVention) could be easily navigated through the left middle temporal and left angular veins. However, the presence of an acute angle between the left supraorbital vein and the left superior ophthalmic vein at their junction (Fig. 1B) hindered further advancement into the left superior ophthalmic vein. The pre-shaped S microcatheter (SL-10 Pre-shaped S) also did not work. Conversely, the angle between the angular and superior ophthalmic veins was obtuse, which enabled a more feasible navigation. A 300-cm microwire (Transend; Stryker Neurovascular) was used to traverse the angular vein, transverse facial vein, and retromandibular vein before ultimately reentering the external jugular vein (Fig. 1C, D). The visibility of the microwire under fluoroscopy facilitated the advancement of a microcatheter, initiated from the external jugular vein. With this guidance, the microcatheter (Prowler 10) and an additional microcatheter (Headway Duo; MicroVention) easily reached the dilated superior ophthalmic vein and a fistulous sac (Fig. 1E). The fistulous sac was embolized using coils and Onyx (Fig. 1F). Complete shunt occlusion was confirmed by a final angiography (Fig. 1G, H).

Case 1: Frontal projection of the right internal carotid arteriogram (A) shows a dural arteriovenous fistula in the right cavernous sinus. The main venous drainage is through an intercavernous sinus to the left superior ophthalmic vein (arrow). The left supraorbital vein (double arrowheads), left angular vein (single arrowhead), and left superior ophthalmic vein (arrow) are connected at the left superomedial orbital rim (asterisk). The volume- rendered image from 3-dimensional rotational angiography (B) shows the acute angle at the junction between the left supraorbital vein (double arrowheads) and the left superior ophthalmic vein (arrow) at the left superomedial orbital rim (asterisk). Single arrowheads denote the left angular vein and the left facial vein. The roadmap image in frontal projection (C) depicts a clear venous drainage path via the left supraorbital vein to the left middle temporal vein, contrary to a less distinct path via the left angular vein to the left facial vein. The microcatheter and microwire (arrowheads) were advanced through the left middle temporal, left supraorbital, and left angular veins. Native image in frontal projection (D) depicts the reentry of the 300-cm microwire (arrowheads) into the retromandibular vein through the transverse facial vein. The roadmap image with the 300-cm microwire in place within the facial and scalp veins (E) guides the second microwire from the left retromandibular vein. Finally, the roadmap in the working projection confirms successful access to the fistula with the second microwire (arrowheads) guided by the 300-cm microwire. Native image in working projection (F) shows Onyx cast and coil mass (arrow) at the fistula. The final right common carotid arteriogram, comprising both native and subtracted images (G, H) in fontal projection, confirms the absence of any residual arteriovenous shunt flow after embolization.
Case 2
A patient in their early 60s presented with proptosis and conjunctival injection. Subsequent MRI suggested the possibility of a CSDAVF. The diagnosis was confirmed by digital subtraction angiography, which revealed a fistulous hole at the posterior superior aspect of the right CS fed by numerous dural feeders on both external carotid arteriograms, showing isolated superior ophthalmic venous drainage (Fig. 2A, B). Thus, endovascular treatment was employed as the first-line approach to treat the lesion.
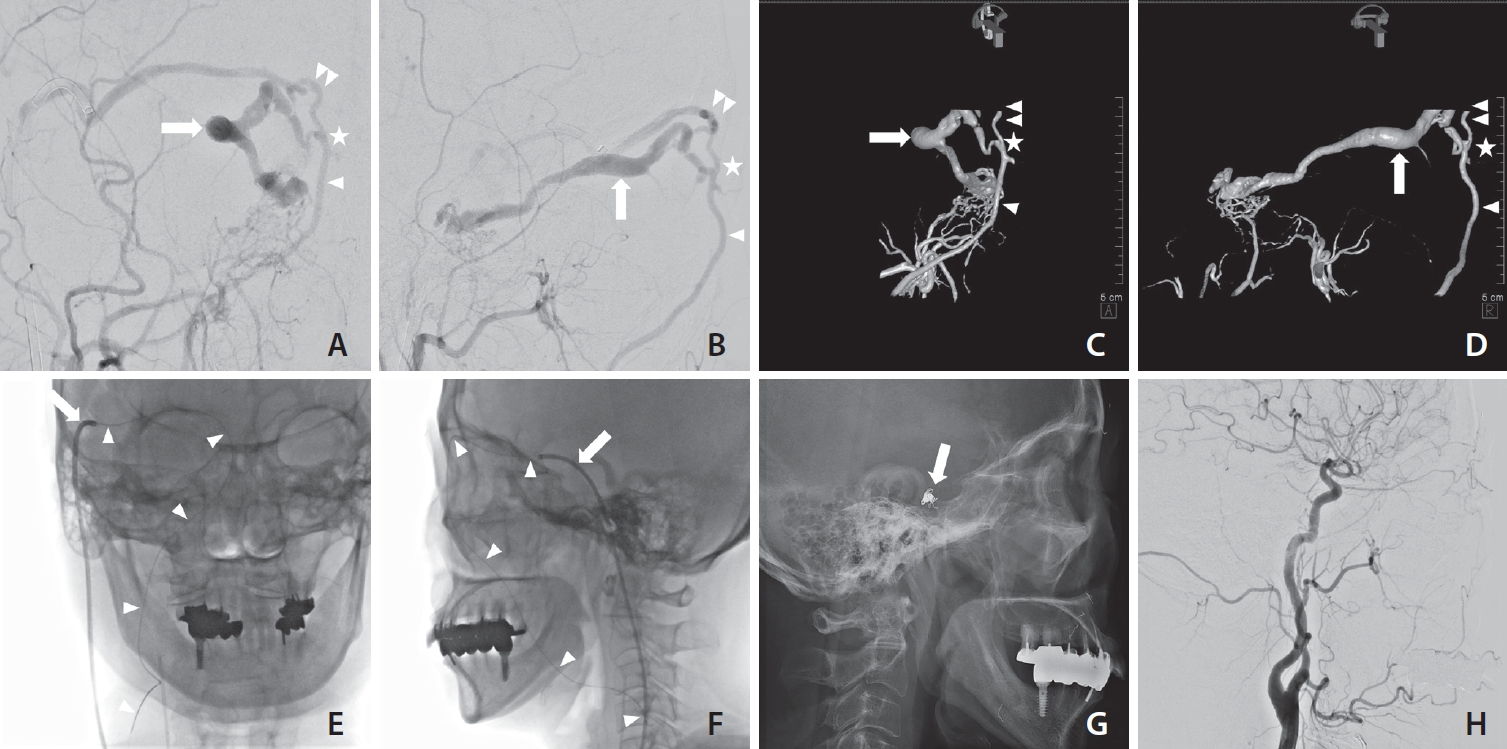
Case 2: Frontal and lateral projections of the right external carotid arteriogram (A, B) depict a dural arteriovenous fistula in the right cavernous sinus. The only venous drainage route is the engorged right superior ophthalmic artery (arrow). The right supraorbital vein (double arrowheads), right angular vein (single arrowheads), and right superior ophthalmic vein (arrow) are connected at the right superomedial orbital rim (asterisks). Three-dimensional rotational angiography (C, D) of the right external carotid artery depicts an acute angle at the junction between the right supraorbital vein (double arrowheads) and the right superior ophthalmic vein (arrows) at the right superomedial orbital rim (asterisks). Single arrowheads denote the left angular vein. Native images in frontal and lateral projections (E, F) show a guiding catheter (arrows) placed in the right middle temporal vein, one of the tributaries of the right external jugular vein, and a 300-cm microwire (arrowheads) placed in the right middle temporal, right supraorbital, right angular, right common facial, and right internal jugular veins. The final right common carotid arteriogram, comprising both native and subtracted images (G, H) in lateral projection, confirms the absence of any residual arteriovenous shunt flow after coil embolization (arrow).
Under general anesthesia and systemic heparinization, a 4-French diagnostic catheter (Jungsung Medical) was inserted into the right external carotid artery through the left femoral artery to obtain a control angiogram and a 6-French guiding catheter (Asahi Fubuki; Asahi Intecc Co., Ltd.) into the right superior vena cava through the right femoral vein. After obtaining the venous phase roadmap image, the guiding catheter was further advanced into the internal jugular vein. Recanalization of the ipsilateral occluded IPS was then attempted, but after several attempts, it was deemed impossible due to complete occlusion. Consequently, the focus was shifted toward the right external jugular vein. An anatomical variation was observed in which the right proximal external jugular vein and the right proximal internal jugular vein were connected. Therefore, it was possible to advance the guiding catheter into the right external jugular vein through the right proximal internal jugular vein. The right middle temporal vein was selected as the main route as it was the most prominent drainage route on angiography. A microwire (Asahi Chikai Black; Asahi Intecc Co., Ltd.) and a microcatheter (Excelsior SL-10, Stryker Neurovascular) were advanced through the right middle temporal vein to reach the right supraorbital vein. It was impossible to navigate further into the superior ophthalmic vein due to the acute angle at the junction with the right superior ophthalmic vein beneath the supraorbital margin of the orbit (Fig. 2C, D). The microwire and microcatheter could go upstream of the right internal jugular vein through the right angular, facial, and common facial veins. The regular microwire was replaced with a 300- cm microwire. The 300-cm microwire was retained, and the microcatheter and guiding catheter were removed (Fig. 2E, F). The existing introducer sheath was removed and replaced with an 8-French introducer sheath with the guidance of the 300-cm microwire. The 6-French guiding catheter was reinserted through the 8-French introducer sheath. After placement of the 6-French guiding catheter in the right internal jugular vein, retrograde navigation of the microcatheter and microwire was achieved with the guidance of the previously inserted 300-cm microwire. Ultimately, catheterization could be performed by entering the superior ophthalmic vein and CS sac. The 6-French guiding catheter was further advanced into the right facial vein to improve proximal support. Embolization using multiple detachable coils was performed, and complete shunt occlusion was confirmed by final control angiography shunt (Fig. 2G, H).
DISCUSSION
We presented 2 interesting cases in which the fistula was successfully occluded in the CS through the dilated superior ophthalmic vein using a facilitating method. Although the draining venous outflow tracts were well visualized on angiogram or roadmap, both cases have proven that access to the superior ophthalmic vein can be challenging.
Several technical challenges are expected. Retrograde navigation to access the superior ophthalmic vein through either the supraorbital or angular vein is challenging. First, accessing the angular vein through the facial vein via retrograde navigation is difficult due to the complex venous tributaries of the facial vein upstream of the common facial vein as well as anatomical variations in the termination of the common facial vein [7]. Second, once retrograde navigation to the supraorbital vein is achieved via the retromandibular and middle temporal veins, further navigation into the superior ophthalmic vein is difficult due to the anatomic complexity of the junction between the supraorbital and superior ophthalmic veins. The anterior portion of the superior ophthalmic vein usually runs slightly backward, medially, and cranially under the orbital roof at the superomedial orbital rim [8]. These anatomical characteristics usually create an acute angle at the junction between the supraorbital and superior ophthalmic veins, thereby precluding successful microwire navigation. Contrarily, the angle at the junction between the angular and superior ophthalmic veins is obtuse. These all indicate that access to the superior ophthalmic vein through the angular vein is easier if we can access the angular vein successfully.
To solve these technical difficulties, we employed a technique that facilitates retrograde facial vein navigation. This facilitating technique involves the use of long microwires, such as a 300-cm microwire, for visible guidance to access the angular vein through the facial vein. Similar to the illustrative cases, the long microwire can be placed along the following veins: external jugular, retromandibular, middle temporal, supraorbital, angular, and facial veins. The use of microwire guidance facilitates access to the angular vein, and the obtuse angle at the junction between the angular and superior ophthalmic vein allows access to the fistula point.
Several considerations should be taken when using this technique. When the long microwire reenters the jugular vein, the latter would either be the internal or external jugular vein based on anatomical variations [7]. In this study, the long microwire reentered the external jugular vein through the transverse facial vein in case 1 and the internal jugular vein through the common facial vein in case 2. Procedural difficulties were not encountered in case 1 as the position of the guiding catheter could be adjusted somewhere in the external jugular vein to deal with both the long microwire and microcatheter. However, this method could not be applied in case 2. In case 2, support and length compatibility were lacking as it was too far to advance the microcatheter into the fistula starting from the proximal internal jugular vein. This problem was solved by using a larger introducer sheath. The guiding catheter was removed while the long microwire was retained. After removing the existing introducer sheath and placing a larger introducer sheath over the retained microwire, the guiding catheter was inserted into the larger introducer sheath parallel to the long microwire. This modification allowed us to advance the guiding catheter into more upstream veins to enhance the support while the retained long microwire facilitated the retrograde venous navigation.
CONCLUSION
For CSDAVF with preferential ophthalmic venous drainage with an inaccessible IPS route, transvenous embolization via the superior ophthalmic vein can be facilitated by a long microwire.
Notes
Fund
None.
Ethics Statement
A case report or case series containing information on less than 3 patients may not require Institutional Review Board (IRB) of Asan Medical Center approval. This article does not include any information that may identify the person.
Conflicts of Interest
YS and DHL have been editors of Neurointervention since 2018 and 2023, respectively. However, they have not been involved in the peer reviewer selection, evaluation, or decision process of this article. No potential conflict of interest relevant to this article was reported. No other authors have any conflicts of interest to disclose.
Author Contributions
Concept and design: DHL. Analysis and interpretation: DHL, YS, BK, and MA. Data collection: BK and MA. Writing the article: BK and MA. Critical revision of the article: DHL, YS, BK, and MA. Final approval of the article: DHL. Overall responsibility: DHL.
