First-Line Aspiration Thrombectomy of M2 Occlusions with a Novel Reperfusion Catheter (REDTM 62): Real-World Experience from Two Tertiary Comprehensive Stroke Centers
Article information
Abstract
Purpose
The direct aspiration first pass technique (ADAPT) is an effective and safe endovascular treatment for distal medium vessel occlusions (DMVOs). We evaluated technical features and initial results of a novel reperfusion catheter (REDTM 62) used for frontline aspiration thrombectomy of M2 occlusions in acute ischemic stroke patients. Appropriate aspiration catheters are crucial for a successful ADAPT maneuver; however, the selection of catheters suitable for smaller-sized vessels is scarce compared to the ones for large vessel occlusions.
Materials And Methods
All patients treated with ADAPT using REDTM 62 as the frontline treatment approach for acute M2 occlusions between December 2022 and February 2024 were retrospectively enrolled. Demographic data, procedural timings and safety, recanalization rates, and outcome data were recorded.
Results
Twenty patients with a median admission National Institutes of Health Stroke Scale (NIHSS) score of 8 were identified. Successful revascularization (DMVO-thrombolysis in cerebral infarction [TICI]≥2b) with REDTM 62 aspiration thrombectomy was obtained in 65.0% (13/20) of cases. The first pass effect was 45.0% (9/20). In 2 cases, the REDTM 62 did not reach the clot due to marked distal vessel tortuosity. Stent retrievers were additionally used in 9 cases and led to an overall DMVO-TICI 2c/3 of 90.0% (18/20). Mean procedural time was 48 minutes. No complications directly related to ADAPT occurred. In-hospital mortality rate was 20.0% (4/20). The median discharge NIHSS score was 2.5. A good functional outcome at discharge (modified Rankin scale 0-2) was achieved in 55.0% (11/20) of cases.
Conclusion
Our initial experiences with the novel REDTM 62 reperfusion catheter for treatment of M2 occlusions is in line with published data. ADAPT using this catheter may be considered as a safe and effective first-line treatment option. Further studies are warranted to validate the initial results.
INTRODUCTION
Distal medium vessel occlusions (DMVOs) account for approximately 25.0–40.0% of acute ischemic strokes (AISs) and may cause significant patient morbidity despite a smaller core infarct volume [1]. Several studies over recent years have shown effectiveness and safety of endovascular recanalization in the distal intracranial vasculature and improved clinical outcomes with successful M2 thrombectomies. Consequently, thrombectomy with aspiration and/or stent retriever (SR) has mostly become the standard of care for patients with M2 occlusions who meet the relevant criteria [2-5].
The direct aspiration first pass technique (ADAPT) has proven to be effective and safe in M2 occlusions using state-of-the-art aspiration catheters. This technique is apparently associated with lower rates of procedural related intracranial hemorrhage compared to SR based thrombectomy [6,7], whereas reperfusion rates and clinical outcomes appear to be similar [8-10].
The choice of the appropriate aspiration catheter is crucial for a successful ADAPT maneuver, especially in DMVOs where an optimized balance between a good catheter trackability allowing a safe and quick access to the occlusion site and the largest possible inner diameter to apply a high suction force is preferable [11]. However, the selection of aspiration catheters suitable for those smaller-sized vessels is scarce compared to the ones for large vessel occlusions (LVOs).
Our purpose was to initially assess technical data, revascularization rates, and outcome data of intentional frontline ADAPT of acute M2 occlusions using a novel reperfusion catheter (REDTM 62 reperfusion catheter; Penumbra, Inc.) in 2 tertiary comprehensive stroke centers. So far, there is no study describing the use of this catheter in endovascular stroke treatment.
MATERIALS AND METHODS
Patients
We retrospectively screened our databases for all AISs patients who underwent frontline aspiration thrombectomy of an acute M2 occlusion with the REDTM 62 catheter over a period of 15 months. The M2 segment was defined as the middle cerebral artery (MCA) branches extending from the genu to the top of the Sylvian fissure and the circular sulcus [12,13].
Inclusion criteria were National Institutes of Health Stroke Scale (NIHSS) score ≥4 or aphasia if the score was <4, no intracerebral hemorrhage (ICH), and absence of established large infarct in the respective M2 territory. Patients were considered eligible for thrombectomy if a functionally and clinically relevant deficit was present and the time window was either within 6 hours or salvageable brain parenchyma based on computed tomography perfusion mismatch was provable. We additionally recorded patient demographic data, clot location, and eligibility for intravenous thrombolysis (IVT).
REDTM 62 Reperfusion Catheter
The REDTM 62 reperfusion catheter is the first catheter of the new RED series. It has received the US Food and Drug Administration clearance in June 2021 and CE mark in September 2022. It has a flexible tip with a distal inner diameter of 0.062” and an extended working length of 138 cm to reach target vessels. It can be used both for frontline aspiration thrombectomy alone and for SR based thrombectomy with simultaneous aspiration.
Evaluation and Outcome Data
Pre-stroke modified Rankin scale (mRS) scores, NIHSS scores at admission and discharge, and mRS scores at admission and discharge were obtained by an experienced stroke neurologist. A good short-term functional outcome was defined as mRS score 0-2 at discharge.
For outcome analysis of the thrombectomy procedure, the following parameters were recorded for each patient: time from symptom onset to groin puncture, time from groin puncture to final recanalization, number of aspiration thrombectomy passes, use of additional bail-out devices, and complications related or not directly related to ADAPT in the medium distal MCA territory. Vessel diameter before the first aspiration attempt was collected using Picture Archiving and Communication System (PACS, JiveX; Visus Health IT GmbH). The transverse diameter of the artery as close to the occlusion site as possible was measured on digital subtraction angiography (DSA) treatment projection. Frontline treatment approach and choice of appropriate thrombectomy devices were at the respective neurointerventionists’ discretion.
Angiographic outcome was assessed independently by 2 experienced neurointerventionists using a modification of the thrombolysis in cerebral infarction (TICI) score for DMVOs [14,15]. We calculated inter-rater agreement using kappa values rating DMVO-TICI values after ADAPT alone and after final DMVO-TICI.
The primary endpoint of this study was successful revascularization of the DMVO, defined as DMVO-TICI score 2b (reperfusion of 50.0–90.0%), 2c (reperfusion of 90.0–99.0%), or 3 (complete reperfusion) of the initially affected territory distal to the target occlusion in the distal MCA territory. Secondary endpoints included safety based on the rate of procedural related complications (ICH according to the Heidelberg Bleeding Classification [HBC] [16], embolism to new territory, and vessel dissection/perforation), first pass effect (FPE), number of aspiration attempts, in-hospital mortality and short-term clinical outcome based on NIHSS, and mRS scores at discharge.
Interventional Procedure
Endovascular treatment was performed under general anesthesia on a biplane angiographic system (Artis Q; Siemens Healthineers). A long sheath (Neuron MAX 088; Penumbra, Inc.) was advanced in the ipsilateral internal carotid artery (ICA) via a transfemoral access and DSA was conducted to confirm the localization and extent of the vessel occlusion(s). Balloon guiding catheters were not used in this cohort of patients.
The REDTM 62 was then advanced to the occlusion site either over a 0.021” microcatheter with a 0.014” microguidewire or over a 0.014” microguidewire alone. The microcatheter and/or microguidewire did not cross the clot. After positioning the catheter tip in the proximal part of the thrombus, the microcatheter and/or microguidewire were removed and the hemostatic valve at the catheter was disconnected to verify that there was no back flow of blood through the catheter (wedging position). Then, aspiration was performed using a suction pump (Medela AXS; Stryker) for at least 3 minutes before slow retraction of the catheter. In case of backward flow inside the catheter, it was left in the cavernous ICA; otherwise, the catheter had to be completely removed applying additional manual suction at the long sheath. A DSA run was performed with standardized settings after each aspiration attempt. A maximum of 2 aspiration attempts were performed. In case of failure of the frontline ADAPT approach (DMVO-TICI 0–2a after aspiration alone), a SR with simultaneous aspiration was used at the neurointerventionist’s discretion.
Statistical Analysis
Qualitative and quantitative data were collected. A median test was used to compare continuous variables. Continuous variables are reported as mean, standard deviation, and range of the lowest and highest values or as median and interquartile range. Categorical variables are reported as number (%). The paired Student t-test and chi-square test were used to compare variables before and after thrombectomy. A P-value <0.05 was considered statistically significant. Inter-rater agreement was calculated using kappa values with Randolph’s free-marginal kappa with a 95% confidence interval (CI). Statistical analyses were performed using SPSS 20.0 (IBM Co.) and SAS 9.2 (SAS Institute).
RESULTS
Patients’ Baseline Characteristics
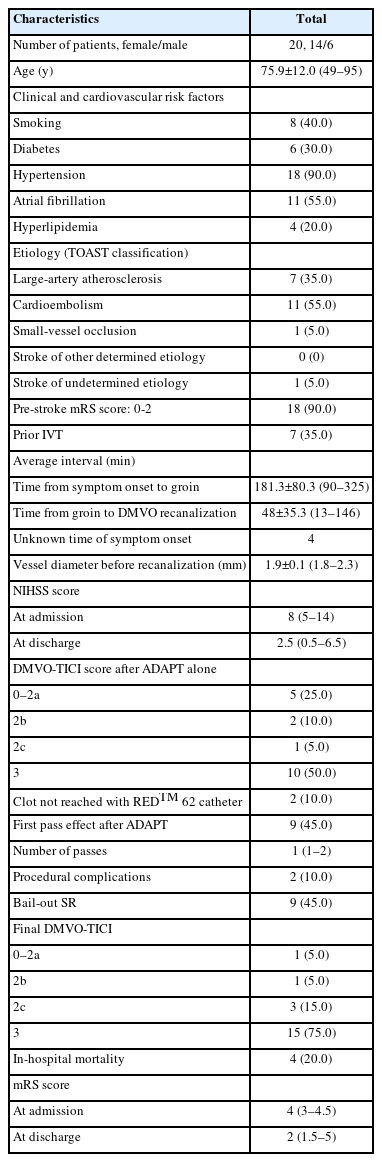
Patients’ baseline characteristics, technical parameters and outcome data are summarized in Table 1 [17]. From December 2022 to February 2024, a total of 468 AIS patients underwent endovascular treatment of an acute intracranial vessel occlusion, 98 of them having M2 occlusions. Twenty patients with an acute M2 occlusion underwent endovascular treatment using ADAPT with REDTM 62 as the first-line intention to treat approach. In total, 70.0% (14/20) of these patients were female, and the mean age was 75.9 years (49–95 y). Overall, 90.0% had a pre-stroke mRS between 0 and 2. The median NIHSS at admission was 8 (5–14). Four patients presented with an unknown time of symptom onset. The mean time between symptom onset and groin puncture in the other patients was 181.3 minutes±80.3 (90–325). Seven patients (35.0%) received bridging IVT. The main stroke etiologies were cardioembolic in 55.0% and atherosclerotic in 35.0%.
Technical Outcomes
The REDTM 62 reached the clot in the M2 segment in 18 cases (90.0%), while in the remaining 2 cases it failed due to marked vessel tortuosity of the respective M2 branch. The pre-occlusive vessel diameter of the M2 branch was 1.9 mm±0.1 (1.8–2.3).
Frontline ADAPT with REDTM 62 resulted in a successful revascularization rate (DMVO-TICI≥2b) of 65.0% (13/20) with a maximum of 2 aspiration attempts and within a mean time of 48 minutes. Complete or near complete revascularization (DMVO-TICI 2c/3) after ADAPT alone was achieved in 55.0% (11/20) of cases. The overall kappa inter-rater agreement while evaluating DMVO-TICI after ADAPT alone was 88.9% with a free-marginal kappa of 0.87 (95% CI, 0.69–1.0). The FPE of ADAPT alone was 45.0% (9/20). The median number of passes was 1 (1–2). SR based thrombectomy was performed just after 1 failed ADAPT attempt in 3 cases with a tortuous MCA anatomy where it was challenging and time-consuming to reach the clot with the REDTM 62 catheter tip. Overall, the frontline ADAPT approach remained unsuccessful (DMVO-TICI 0–2a) in 35.0% (7/20) of cases either due to a maximum of 2 failed attempts (n=5) or due to an inability to reach the clot with the REDTM 62 (n=2). SRs were additionally used in these 7 cases and in 2 cases with a DMVO-TICI 2b after ADAPT alone and led to an overall DMVO-TICI 2c/3 of 90.0% (18/20). Overall, kappa inter-rater agreement of the evaluation of final DMVO-TICI values was 95.0% with a free-marginal kappa of 0.94 (95% CI, 0.82–1.0).
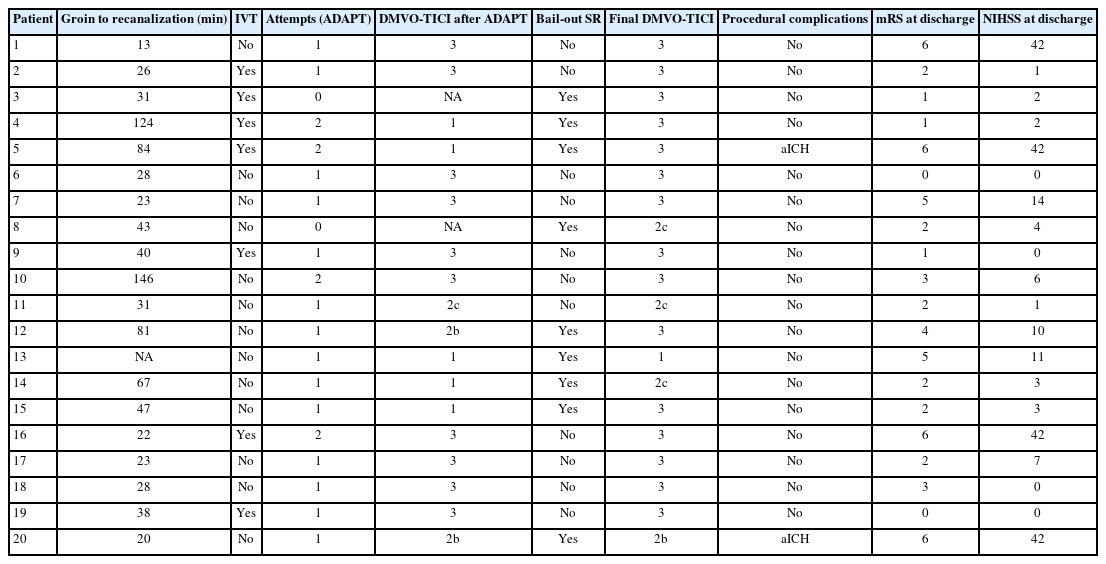
The mean overall recanalization time was 48 minutes±35.3 (13–146). No complications directly related to ADAPT occurred in our cohort of patients. Two class 3c ICHs according to HBC were observed after unsuccessful ADAPT and subsequent complete recanalization with SR thrombectomy. Distal emboli, embolism to a new territory, and vasospasm equally were not encountered in our collective. Technical parameters and clinical outcome are listed in detail in Table 2. Fig. 1 demonstrates an illustrative case of an acute left M2 occlusion treated with frontline ADAPT using REDTM 62.
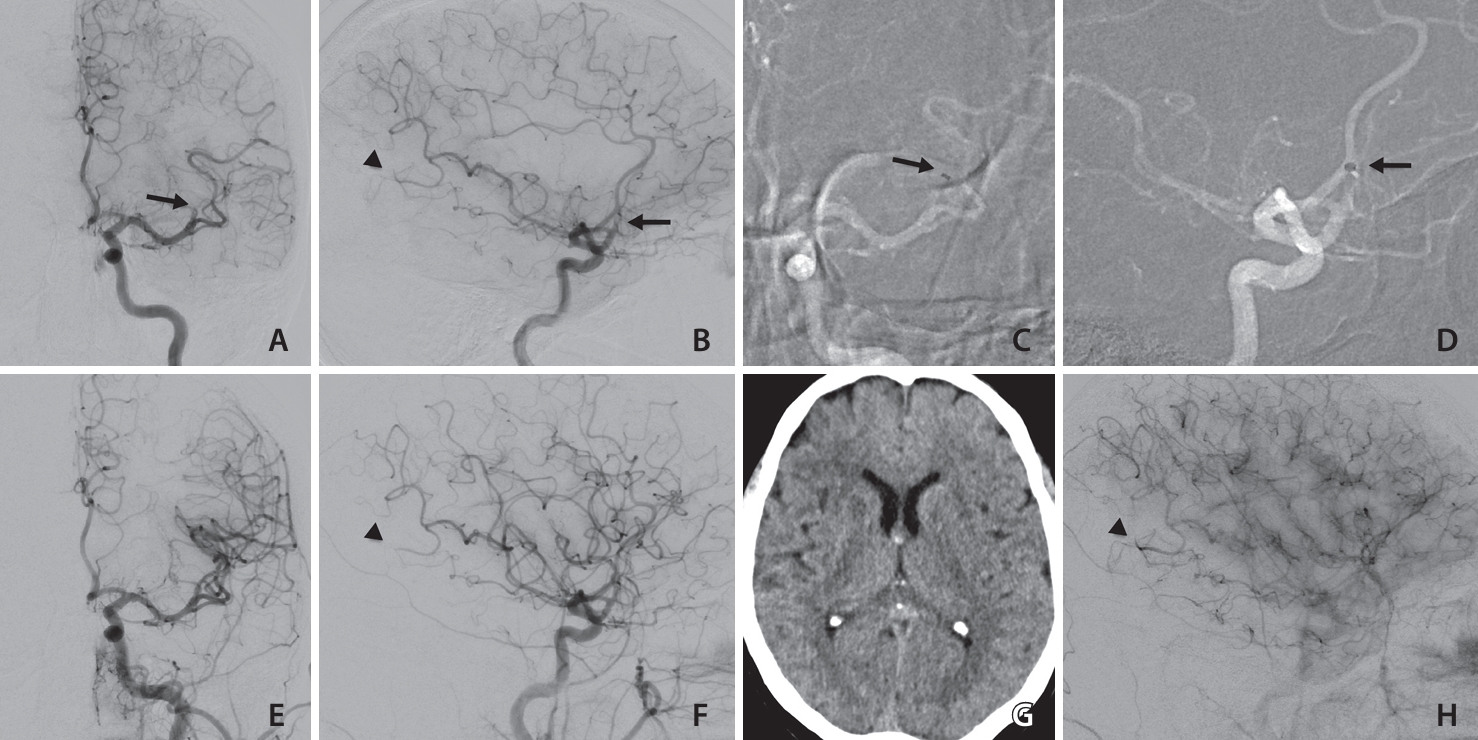
Middle aged patient with an acute left superior trunk M2 occlusion (arrows in A, B). National Institutes of Health Stroke Scale (NIHSS) 5 at admission, 2 hours from symptom onset, pre-stroke modified Rankin scale (mRS) 1. A direct aspiration first pass technique with REDTM 62 (Penumbra, Inc.) (first pass) led to distal medium vessel occlusion thrombolysis in cerebral infarction 3 (E, F; arrows in C, D indicate catheter tip). No infarction on 24 hours follow-up cranial computed tomography (G). NIHSS 0 and mRS 1 at discharge. Note concomitant distal dorsoparietal M4 occlusion (arrowheads in B, F, H).
Clinical Outcomes
The median NIHSS improved from 8 (5–14) at admission to 2.5 (0.5–6.5) at discharge. The median mRS was 4 at admission and 2 at discharge. In total, 55.0% of patients (11/20) achieved a good short-term functional outcome (mRS 0-2). In-hospital mortality was 20.0% (4/20). One patient with a successfully recanalized primary M2 occlusion of the superior trunk had a concomitant primary M3 occlusion in the inferior trunk. First-line SR thrombectomy of this distal occlusion led to a symptomatic ICH in the territory of the inferior trunk and resulted in the patient’s death. One patient with a pre-stroke mRS of 3 and 2 patients with a pre-stroke mRS of 2 died from pulmonary insufficiency during hospitalization (Table 2).
DISCUSSION
Our initial experiences at 2 centers with the new REDTM 62 aspiration catheter replicate the results of the ADAPT technique in DMVOs. It appears to be a safe and efficient catheter for frontline aspiration thrombectomy of acute M2 occlusions.
Recent retrospective and prospective studies have shown the clinical effectiveness of endovascular stroke treatment beyond the level of proximal LVOs and for the anterior circulation. The proven benefit of LVO thrombectomies seems to be transferable to M2 occlusions [18]. Occlusions of medium and distal vessels account for 25.0–40.0% of all brain vessel occlusions and may lead to severe neurological deficits. This applies in particular to M2 occlusions, and thus adequate stroke treatment has a significant clinical importance for these occlusions [1,19].
With the ongoing development of easily navigable largebore aspiration catheters, the ADAPT has become a well-established thrombectomy technique for endovascular stroke treatment in general [7,20,21]. In recent years, several retrospective studies on M2 occlusions reported no statistically significant differences between aspiration thrombectomy and SR based thrombectomy in terms of reperfusion rates and clinical outcome. Moreover, ADAPT seems to be associated with less procedural-related intracranial hemorrhages compared to SR thrombectomy [5-7].
Most studies focusing on frontline ADAPT of M2 occlusions used either aspiration catheters with small inner diameters, mainly the Penumbra 3MAX (0.035”) and 4MAX (0.041”) catheters [22-25] or larger-bore catheters such as SOFIA 5 Fr (0.055”) or Catalyst 5 Fr (0.058”) [8,13,26]. The latter 2 have also smaller inner diameters than the REDTM 62. Usually, smaller catheters are characterized by a better trackability compared to the ones with larger diameters which is important for an atraumatic advancement to the occlusion site, especially in the distal intracranial vasculature. On the other hand, the larger the catheter tip diameter, the greater the applied suction force. It is assumed that an undersized aspiration catheter diameter might be one reason for failed aspiration thrombectomy maneuvers in general. Consequently, an optimal ratio of vessel size to aspiration catheter diameter is considered to be essential for a successful ADAPT approach. However, thrombus length and clot composition might also affect the recanalization rates of ADAPT [11,27] Moreover, the optimal aspiration force to engage the thrombus and avoid a vessel collapse and/or vessel injury is still controversially discussed for LVOs and is not necessarily transferable to smaller-sized distal medium vessels [13]. The new REDTM 62 aspiration catheter with a 0.062” inner diameter is designed to navigate complex distal vessel anatomy and to deliver powerful aspiration even in challenging anatomy [28]. The goal of this retrospective study was to focus on its effectiveness in the treatment of M2 occlusions as the selection of aspiration catheters suitable for those smaller-sized vessels is scarce compared to the ones for LVOs. To the best of our knowledge, no previous cases of frontline ADAPT with REDTM 62 have been described in the literature.
With REDTM 62 frontline ADAPT of acute M2 occlusions, a successful recanalization (DMVO-TICI≥2b) was achieved in 65.0% of cases (13/20) with 55.0% (11/20) DMVO-TICI 2c/3 results. The first-pass DMVO-TICI 2c/3 was 45.0% (9/20). In a study of M2 aspiration thrombectomies using mainly SOFIA 5 Fr distal access catheters as first-line treatment approach, Grieb et al. [26] reported higher successful recanalization (TICI≥2b) rates in 86.5% though with comparable TICI 3 rates (61.5%). Romano et al. [13] used the Catalyst 5 Fr for frontline ADAPT of acute M2 occlusions and reported initial results comparable to our results with TICI≥2b in 8 of 11 patients (72.7%) and a first-pass TICI 3 in 5 of 11 patients (45.5%). Park and colleagues [29] achieved higher TICI≥2b rates in 84.0% of cases in their series of M2 occlusions treated with the 4MAX catheter; however, complete recanalization was only achieved in 47.0% of cases. Hence, our 2 center study in a real-world setting is overall in line with these previously published data of M2 thrombectomies treated with ADAPT using different aspiration catheters. However, angiographic outcomes of DMVOs treated with aspiration thrombectomy using the 3MAX varies considerably in the literature with TICI≥2b rates between 59.5% and 83.9% [22,23]. For those cases, an additional intermediate catheter placed more proximally to provide better support to the system is usually needed.
If effective recanalization cannot be achieved with the ADAPT technique, a SR can easily be navigated through the REDTM 62. In our cohort of patients, 9 patients underwent additional SR based thrombectomy either after failed ADAPT or following DMVO-TICI 2b after ADAPT alone. Complete or near complete recanalization was achieved in 7 of them. Thus, the overall DMVO-TICI 2c/3 rate was 90.0% (18/20). ADAPT and SR based thrombectomy techniques should be seen as complementary techniques. M2 occlusions after a sharp vessel angulation in particular can be very challenging to catheterize with a distal access catheter. We experienced 2 cases in which the thrombus in the M2 branch could not be reached by the catheter tip due to vessel tortuosity. Both cases were recanalized with a SR.
However, for a reliable evaluation of an aspiration catheter and the appropriate ADAPT technique, recanalization success alone is not sufficient. A high procedural safety with a low complication rate is crucial for a careful risk-benefit analysis [30], particularly in smaller, fragile medium sized vessels. Here, deployment and retrieval of a SR is said to increase the risk of traction injury to smaller arterioles with potential symptomatic subarachnoid hemorrhage [31]. We did not observe any major complications attributable to ADAPT with the REDTM 62. This is line with published data about ADAPT in M2 occlusions using SOFIA 5 Fr or Catalyst 5 Fr where major complications were equally not observed [8,13,26]. However, emboli to new territory after ADAPT with the Catalyst 5 Fr in up to 9% of cases [8,13] and asymptomatic ICHs (aICHs) following ADAPT with the SOFIA 5 Fr in 3.9% of cases have been reported [26]. We encountered 2 aICHs (Class 3c according to HBC), both after bail-out SR thrombectomy of a M2 occlusion following failed ADAPT. Thus, it is as yet unclear whether this complication is related to the ADAPT maneuver or rather to the SR maneuver.
Our study has limitations. The retrospective design can be regarded as the main limitation. We used a new device for aspiration thrombectomy; thus, the number of patients is small. During the study period, different thrombectomy devices were available in both centers, and the respective treatment strategy and use of REDTM 62 was up to the discretion of the neurointerventionist and might therefore lead to a selection bias. Only patients who underwent thrombectomy of a M2 occlusion with frontline ADAPT using REDTM 62 were included. Thus, there has not been a consecutive enrollment of patients with M2 occlusions. Acute M2 occlusions that were intentionally treated with other thrombectomy techniques/devices (e.g., SR based techniques) as frontline therapy were excluded. None of the angiographic or clinical outcomes were core lab adjudicated. Apart from that, certain inhomogeneities within the cohort of patients must be taken into account with regard to postinterventional clinical development. Underlying cardiovascular risk factors and comorbidities might have a considerable impact on clinical outcome; thus, clinical outcome might not be directly consistent with the use of the REDTM 62. However, exact records of various comorbidities and clinical factors are not available for all patients due to the retrospective design.
CONCLUSION
Our initial experience at 2 centers with the novel REDTM 62 reperfusion catheter for treatment of M2 occlusions in AIS patients is in line with published data. This catheter may be considered as safe and effective for first-line ADAPT of acute distal MCA occlusions. More data is needed to validate the initial results and prospective studies are warranted to compare the safety and efficacy of the REDTM 62 to other aspiration catheters suitable for first-line aspiration thrombectomy of M2 occlusions.
Notes
Fund
None.
Ethics Statement
Approval was obtained from the local Ethical Review Board, Aerztekammer Nordrhein, for this retrospective study (number 169/2023). The study was performed in agreement with institutional guidelines and with the ethical standards according to the latest version of the Declaration of Helsinki. Due to the retrospective design of the study, a separate informed patient consent was not required.
The consent for publication is not required as the submission does not include any images or information that may identify the person.
Conflicts of Interest
The authors have no conflicts to disclose.
Author Contributions
Concept and design: DG, KS, HL, MSH, and FB. Analysis and interpretation: DG, KS, HL, MSH, and FB. Data collection: DG, HW, KS, CL, MSH, and FB. Writing the article: DG and FB. Critical revision of the article: HW, KS, CL, HL, MSH, and FB. Final approval of the article: DG, HW, KS, CL, HL, MSH, and FB. Statistical analysis: DG and FB. Overall responsibility: DG.