Mechanism of Procedural Failure Related to Wingspan
Article information
Abstract
Purpose
Wingspan is the only FDA approved self-expanding stent for intracranial artery and known to have better delivery compared to balloon expandable stent. However, some delivery failure has been reported but incidence and mechanism of the failure have not been completely elucidated. We present the cause and mechanism of Wingspan deployment failure experienced in our Institute.
Materials and Methods
We experienced deployment failure in seven patients (8.8%) out of 80 patients who underwent Wingspan stenting since 2007. Mean age of the patients was 62 (range 47~78) and male to female ratio was 6:1. We evaluated the cause and mechanism why the deployment was not successful and how we could manage it subsequently.
Results
We categorized failures occurred in seven patients into three categories: delivery failure (n = 3), deployment failure of stent (n = 3), retrieval failure of dual tapered (olive) tip of the inner body through the deployed the stent (n = 1). The technical failure in using Wingspan stent (delivery, deployment and retrieval failures) are related to tortuousness of the proximal (n =4) as well as distal (n =1) cerebral vessels to the stenotic lesion and bulky profile of the olive tip (n =2).
Conclusion
The technical failure in using Wingspan stent (delivery, deployment and retrieval failures) are related to tortuousness of the proximal as well as distal cerebral vessels to the stenotic lesion and bulky profile of the olive tip. To avoid device-related complication, complete understanding of the stent design is mandatory before using the stent.
Manifestation of atherosclerosis is known to be various according to ethnic difference [1-6]. Atherosclerotic intracranial stenosis is more common in Koreans than western countries [5]. Bare metal stent for coronary artery has been used effectively in Korea, although the stent was only used as an investigational purpose in the United States [3, 7-10].
The only stent approved by the Food and Drug Administration for the treatment of intracranial atherosclerotic disease is the self-expanding Wingspan stent system (Stryker, Kalamazoo, MI, USA). It has been available since 2005 for the treatment of patients with 50 to 99% stenosis who had had a transient ischemic attack or stroke while receiving antithrombotic therapy [11]. It has also been used in stent-assisted coil embolization for aneurysms in case of atherosclerotic narrow of parent arteries [12].
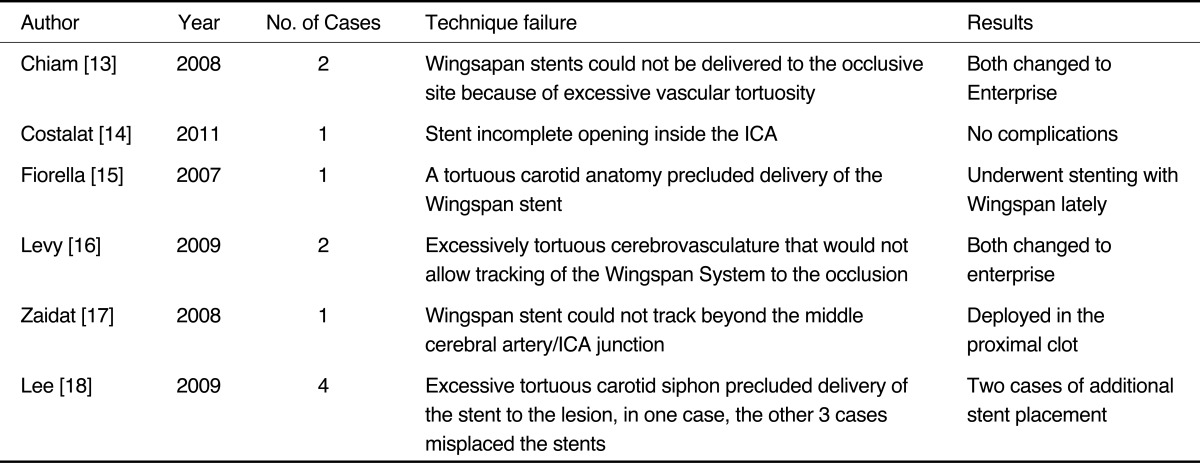
Although some delivery failure has been reported (Table 1), there were few literatures to introduce failure rate of the Wingspan stent deployment and the mechanism of the failure [13-18]. We report deployment failure of Wingspan stent in our experiences and present mechanism of the failure and how to manage the failure.
MATERIALS AND METHODS
The database of neurointervention in Asan Medical Center (AMC) was reviewed retrospectively to identify all Wingspan stent procedures which were used for the treatment of intracranial atherosclerotic disease. Records were reviewed to identify cases of failure of stent deployment in daily practice.
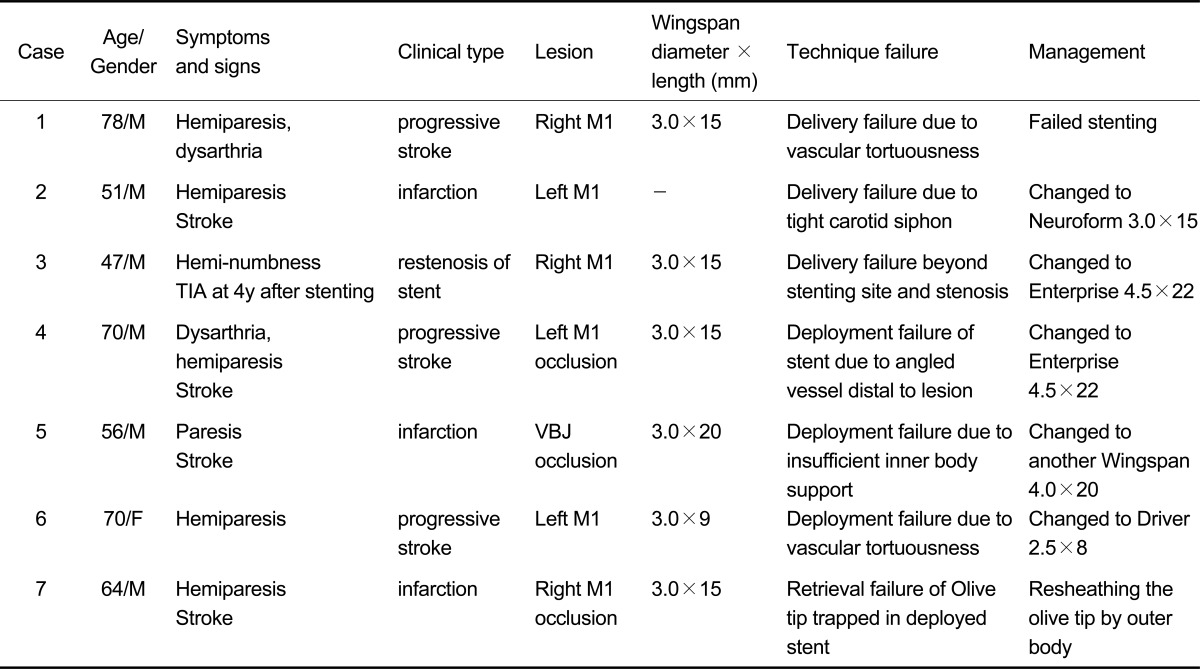
Since 2007, 80 Wingspan stents were placed in our department for the treatment of intracranial atherosclerotic arterial stenosis. Procedural details are the same as those described previously [3, 7-9, 19]. Among 80 patients, we identified seven instances (8.8%) of failure of stent deployment (Table 1). Mean age of the patients was 62 (range 47~78) and male to female ratio was 6:1.
We excluded a patient because Wingspan was used for an aneurysm coil embolization. In this patient, Wingspan was inappropriately deployed proximal to the target lesion while treating a wide-necked paraclinoid internal carotid artery (ICA) aneurysm with atherosclerotic change in parent artery. A Neuroform Ez (Stryker, Kalamazoo, MI, USA) was used for stent-assisted coil embolization after the Wingspan stent was removed by a snare loop device successfully.
We defined procedural failure as failure of any process in Wingspan stent insertion, delivery failure as failed delivery of Wingspan system into proper position for stenotic lesion, deployment failure as failed deployment of stent despite proper positioning of Wingspan system, and retrieval failure as failed retrieval of dual tapered (olive) tip after deployment of the stent because of the friction between stent strut and bulky olive tip.
Wingspan Delivery System
Wingspan delivery system consists of inner and outer bodies, and nitinol (Wingspan) stent. When the delivery system is introducing, a olive tip protrudes distal to the outer body which has outer diameter of 3.5F. Dual tapered tip has 9 mm length, entry profile of 0.027 and mid-profile of 0.046 inch. When the stent is being deployed, outer body is pulling back while maintaining the inner body in its own position. After deployment, dual tapered tip is retrieved by pulling the delivery system through the deployed stent.
RESULTS
We categorized procedural failures occurred in seven patients into three categories (Table 2): delivery failure of the system (n = 3), deployment failure of stent (n = 3), retrieval failure of olive tip of the inner body through the deployed the stent (n = 1).
Delivery Failure
There were three patients in whom delivery of the delivery system to the lesion has failed. In patient 1, while treating a serious stenosis at right M1-M2 junction, successful balloon angioplasty was performed but the Wingspan stent delivery system could not be introduced to the lesion because of excessive vascular tortuousness. We failed to deploy the stent despite multiple attempts. In patient 2, we could not advance the stent delivery system to the target lesion beyond the tight carotid siphon even after using stiff guide wire while treating a focal severe stenosis at middle portion of left middle cerebral artery trunk. A Neuroform stent then was used as a substitute after balloon angioplasty. Patient 3 revealed a severe stenosis of the right M1 segment just distal to the previously stented area by bare metal stent in which there was no restenosis. The olive tip of the delivery system could not introduce beyond the previous stent after balloon angioplasty. Then an Enterprise was used to relieve the stenosis.
Deployment Failure
As in three patients of our experience, there seemed to be different mechanism of deployment failure. In patient 4, the angiogram showed complete occlusion of the distal left M1. The stent was not deployed even though the stent delivery system was in proper position to cover the lesion. We removed the whole system because there was too much resistance felt in the outer body, which was not pulling back smoothly. After removal of the stent, we found that there was partially deployed stent at the tip (Fig. 1). This configuration revealed that the acute angulation between M1-2 segment prevented continuous and smooth deployment of the stent. Finally, we introduce an Enterprise and could open the occluded segment. In patient 5, stent delivery system was finally advanced to the basilar artery through excessively tortuous right subclavian artery and vertebral artery, but the stent could not be deployed because the stabilizer was not as stiff as to provide enough supporting force. Then we had to try another Wingspan stent and made the success finally. As to patient 6, stent could not be deployed at the proper position because of marked resistance between inner and outer bodies caused by excessive proximal vascular tortuousness, even the olive tip of the delivery system had navigated over the lesion. We tried to advance the stent by pushing the inner body but finally failed to push the stent segment because olive tip at the end of the inner body was stretched out from the end of the outer body (Fig. 2). When the delivery system was withdrawn, we found that the stretched portion of the inner body was exposed far beyond the stent loaded segment in the delivery microcatheter (outer body).
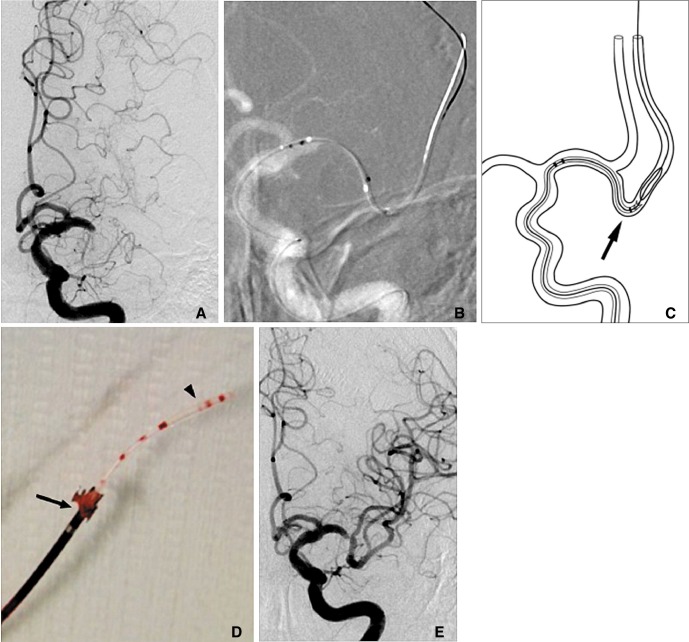
A 70-year-old male patient presented with dysarthria and hemiparesis due to left M1 occlusion.
A, B. Wingsspan delivery system was introduced into the occluded left middle cerebral artery (MCA). However, outer body could not been pulled back to deploy the stent because there was excessive resistance between inner and outer body of the delivery system.
C. Diagram shows the mechanism when and how the deployment failure happened. Note an acute angled bending of the inferior division of M2 (arrow).
D. Removed system showed that partially deployed the stent tip (arrow) in between outer body and stretched dual tapered (olive) tip (arrowhead).
E. Final angiogram shows rather good filling of the MCA branches after deployment of an Enterprize stent.
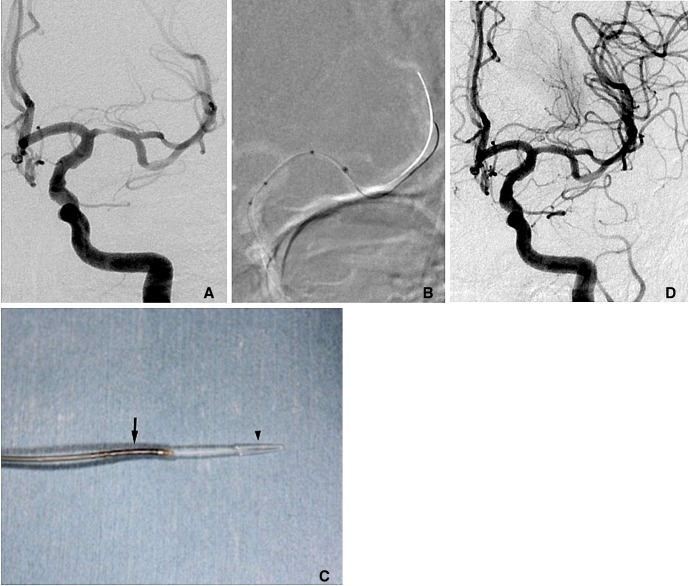
A 70-year-old female presented with dysarthria and right sided weakness.
A. There was severe stenosis of right M1 and the proximal cervical internal carotid artery was tortuous (not shown).
B. Wingspan was delivered in proper position without successful deployment of the stent due to marked resistance between inner and outer body.
C. Removed system reveals stretched inner body and olive tip (arrowhead) protruded far beyond the loaded stent segment (arrow) which was not introduced at all.
D. Final angiogram obtained after Bare metal stent deployment reveals good patency of the lumen and distal branch filling.
Retrieval Failure of the Dual Tapered (Olive) Tip
As in patient 7, after successful deployment of Wingspan stent, we met a little resistance when we tried to retrieve the olive tip of the stent delivery system. The outer body was readvanced through the deployed stent and then the olive tip was retrieved and repositioned to the distal end of the microcatheter (outer body). Reducing the size gap between olive tip and inner body shaft can make better smooth retrieval of the delivery system.
DISCUSSION
The published data on the use of the Wingspan stent for intracranial atherosclerosis revealed that technical success rate was high between 96.7% and 98.8% [15, 17, 18, 20]. When we review the literature, there were only few publications regarding Wingspan deployment failure [13-17] being totally less than one dozen of cases. We reported seven cases of Wingspan stent deployment failures in our experience and revealed 7.5% failure rate except the last patient in whom stent deployment was finally successful.
The overall rate of technical failure in our study seems to be higher than other studies. This difference may reveal that the failure rate can be underestimated because information regarding stent deployment failure is not exactly reported. The other possible reason is that some studies did not include stent misplacement as technical failure [18].
The main cause of Wingspan stent delivery failures in the published studies was excessive cerebral vascular tortuousness [21]. There were several reported cases of Wingspan delivery failure because of excessively tortuous cerebrovasculature [13, 15-17]. Among them, a patient presented later with recurrent stenosis and successfully underwent stenting with Wingspan [15].
Although vascular tortuousness was the delivery failure reason as in two out of three delivery failure patients, we experienced in a patient whom the olive tip of the stent could not pass the lesion beyond the previously stented M1. This passage failure of the olive tip is due to 0.046 inch (1.17 mm) mid-profile of the olive tip could not pass the rigid tube of previous bare metal stent as in patient 3.
The salvage technique for the delivery failure is to resort to stent with more flexible delivery system and thinner profile, such as Enterprise and Neuroform. Such self-expanding stents designed for coiling of wide-neck aneurysm sometimes neither have proper size of stent length and diameter nor enough radial force to resist delayed restenosis in atherosclerotic lesions. Lesley et al. [22] introduced a catheter exchange technique for the Wingspan stent deployment by cutting off the olive tip of the delivery system if the delivery system could not be advanced to the lesion. This concept is similar to use Neuroform except that outer diameter of the delivery catheter is 2.8F in high-flow renegade for Neuroform compared to 3.5F in the outer body for Wingspan.
Although delivery failure was the main mechanism as in 3 out of our seven patients, we also met deployment or retrieval failure which has not been described in detail previously. Three stent deployment failures were related to different reasons. Two of them occurred due to proximal vessel tortuousness and the other occurred due to angled vessel configuration just distal to the stenotic lesion. Acute distal vessel angle as in M1-2 junction probably made the olive tip buckled and precluded smooth stent deployment. Two other cases revealed that the stent might not be delivered because of insufficient support of the inner body system in one and a part of the inner body had been pushed out of the delivery microcatheter (outer body) without introducing the stent segment in the other.
Retrieval failure of the olive tip did not lead to procedure failure because we could finally remove the system after resheathing the inner body by advancing the outer body over the inner body up to the olive tip. Even though this failure can be managed by resheathing technique, incomplete understanding of the stent design might result in injury of the stent vessel by forceful pulling of the system despite the resistance of the olive tip against deployed Wingspan stent. Less experience of the operators is also one reason of stent deployment failures. Lee et al. [18] reported three cases of stents misplacement in the early phase of their experience.
In conclusion, our study revealed that there were three mechanisms of technical failure in using Wingspan stent: delivery, deployment and retrieval failures. These technical failures are related to tortuousness of the proximal as well as distal cerebral vessels to the stenotic lesion, rather large and bulky profile of the olive tip, tight and rigid lumen of previously stented vessel. To avoid device-related complication, complete understanding of the stent design is mandatory before using the stent.