Balloon-Assisted Coil Embolization and Balloon Angioplasty for Post Subarachnoid Hemorrhage Vasospasm: Initial Experience with Scepter Mini Balloon
Article information
Abstract
The scope of this technical note is to report our experience with balloon remodeling for wideneck aneurysms and balloon angioplasty of post-subarachnoid hemorrhage vasospasm using the novel Scepter Mini balloon (SMB). Five cases were treated with balloon remodeling for aneurysmal subarachnoid hemorrhage, 2 of which were additionally treated with angioplasty due to post-bleeding vasospasm. All patients had their aneurysm located on parent vessels with a diameter smaller than 2 mm. Complete occlusion was noted in all aneurysms, and the patients had no short-term complications attributed to the catheterization. Additionally, we confirm the previously reported smooth navigation of the balloon through vessels with tortuous anatomy without catheter-induced vasospasm. Based on our experience, the SMB can be a safe and efficient device for applying the balloon remodeling technique for distally located wide-neck aneurysms and distal balloon angioplasty.
INTRODUCTION
The balloon remodeling technique was first introduced in the late 90’s [1], revolutionizing the endovascular management of wide-necked intracranial aneurysms. The technique is based on the inflation of a non-detachable balloon into the parent artery across the aneurysm neck, while coil deployment is performed through an additional catheter. The main difference between the technique compared with stent-assisted coiling is that the balloon is eventually removed at the end of the procedure, thus avoiding the risks linked to stent placement [2]. Balloon angioplasty is often performed for symptomatic vasospasm following aneurysmal subarachnoid hemorrhage [3].
One newly released balloon catheter is the Scepter Mini balloon (SMB), which obtained US Food and Drug Administration approval in 2019. The SMB has been introduced as a novel dimethyl-sulfoxide compatible dual lumen balloon catheter. With a 1.6 French (Fr) distal tip and a 2.2 mm balloon at the nominal diameter, the SMB is the lowest profile compliant double-lumen balloon, and it provides better navigability with better distal arterial branch access. The SMB was initially introduced with indications similar to its predecessors, the Scepter C and XC catheters. The SMB showed promising results for transarterial balloon-assisted embolization of dural arteriovenous fistulae (dAVFs) and cerebral arteriovenous malformations (cAVMs) using liquid embolic agents [4], allowing a safer and more efficacious delivery of Onyx into smaller, more distal, and tortuous arterial feeders.
We report our experience with balloon remodeling for wide-neck aneurysms and balloon angioplasty of post-subarachnoid hemorrhage (SAH) vasospasm using the novel SMB.
MATERIALS AND METHODS
Five patients with a ruptured cerebral aneurysm underwent endovascular treatment with the balloon remodeling technique between 2020 and 2021 with the SMB. Two of these patients underwent balloon angioplasty for symptomatic vasospasm with the SMB. The balloon remodeling technique was performed for the treatment of anatomically difficult aneurysms, particularly those with a wide neck. This technique was chosen in order to achieve higher occlusion rates. Moreover, in case of an intraprocedural rupture, which is a major complication, the balloon could be immediately inflated to control bleeding without clinical consequences. The risk of intraprocedural rupture is higher in very small aneurysms (less than 3 mm), which applies to all of the included cases.
All patients had aneurysmal hemorrhage (4 subarachnoid hemorrhages and 1 intraventricular). All procedures were performed under general anesthesia using a transfemoral approach, and no distal access catheter was used. The balloon-related lumen and the balloon itself were flushed and filled with pure contrast agent, and subsequently deflated in saline before the SMB was used according to the manufacturer’s instructions [5]. A 6 Fr Neuron Max 088 (Penumbra Inc., Alameda, CA, USA) guiding catheter was utilized in all cases. Instead of a 0.01-inch, the Hybrid 0.008- and 0.007-inch (Balt Extrusion, Montmorency, France) microwires were used for navigation of the SMB to avoid a catheter-induced vasospasm due to the small diameter of the arterial branches. The diameter of the parent arteries did not exceed 2 mm in all cases. Follow-up modified Rankin scale (mRS) scores were obtained at 6-months post-intervention.
Written consent for using their data for research purposes was obtained in all included cases according to institutional guidelines, and the study was approved by the Institutional Review Board.
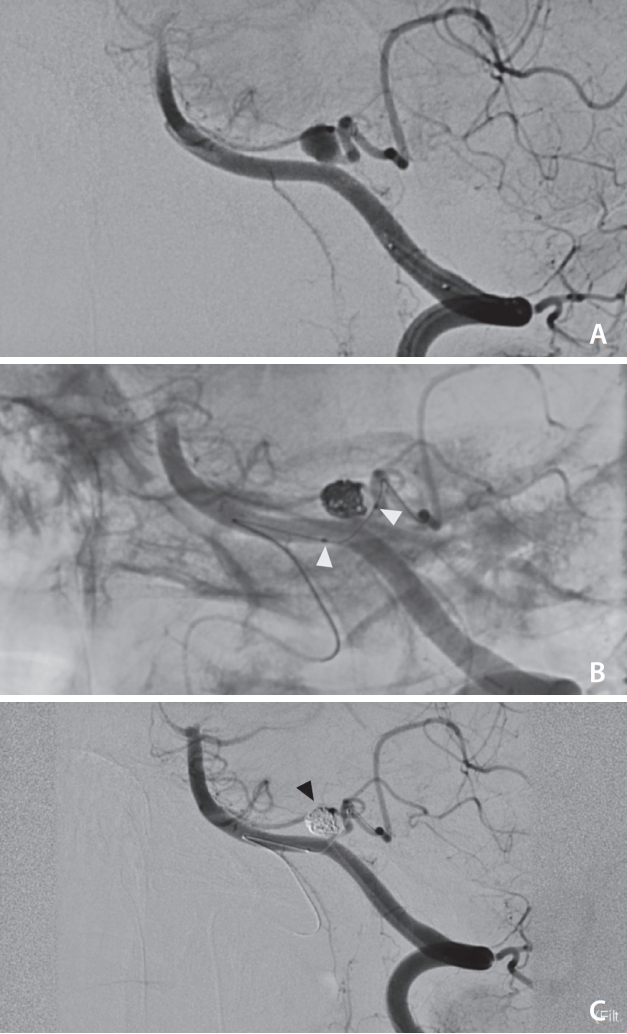
RESULTS
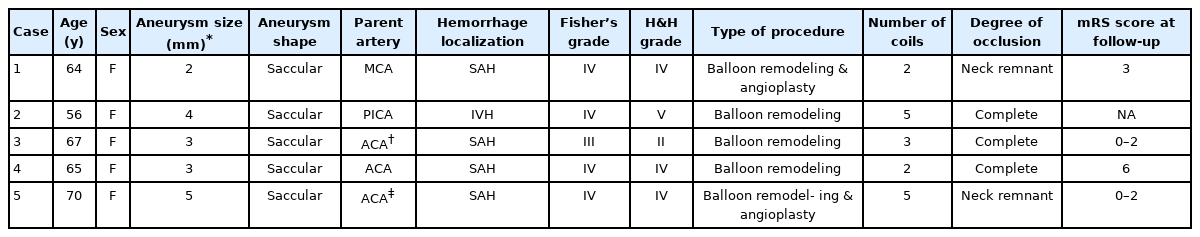
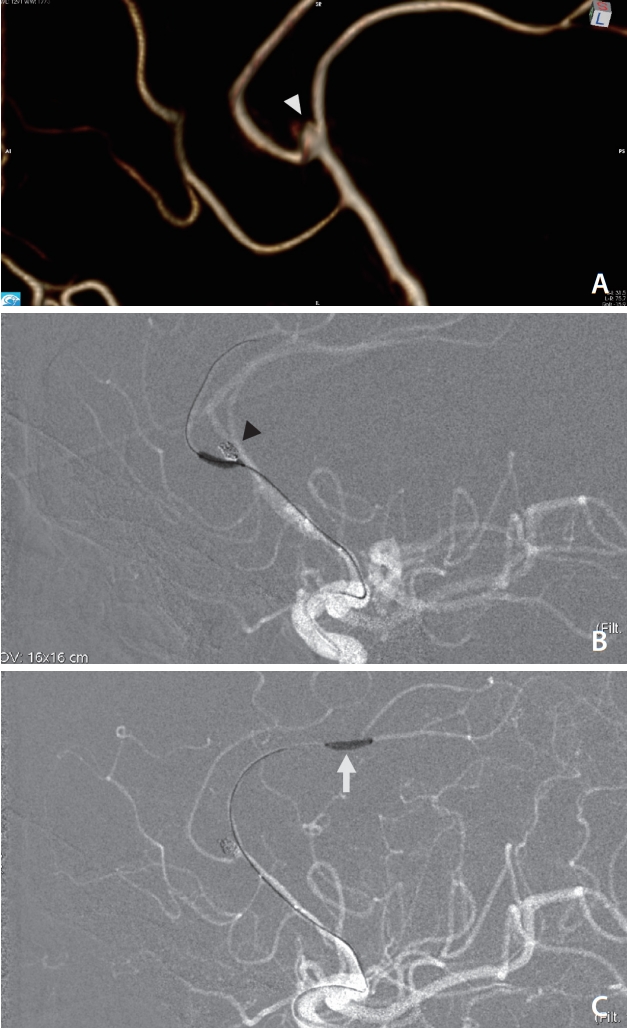
Five patients were treated for aneurysmal hemorrhage (4 subarachnoid hemorrhages and 1 intraventricular). The patients were all female, and the mean age was 58 years. Three of the aneurysms were located distally in the anterior cerebral artery, 1 was a distal aneurysm of the inferior trunk of the right middle cerebral artery, and 1 was a posterior inferior cerebellar artery (PICA) aneurysm. The characteristics of each case are presented in the Table 1.
The intended use of the SMB was successful in all cases. The balloon was successfully navigated and advanced easily in distal branches, and the balloon remodeling technique or balloon angioplasty was performed without complications related to the intervention. Interestingly, no catheter-induced vasospasm was seen, even in small distal branches. Follow-up was recorded in 4 out of 5 patients, with 2 patients having a favorable clinical outcome (mRS score 0–2), 1 patient presenting with mild dependency (mRS score 3), and 1 patient eventually passing away due to complications related to the long-term stay at the intensive care unit (Table 1). The patients’ angiographic images at follow-up were not available. Example cases are shown in Figs. 1 and 2.
A 70-year-old female (case 2) presenting with aneurysmal SAH (Hunt and Hess grade IV) from rupture of a left wide-neck pericalossal aneurysm (A, white arrowhead). The patient was treated endovascularly with balloon remodeling with a Scepter Mini balloon (SMB) on the 8th post-bleed day. The balloon was successfully inflated at the origin of the calossomarginal artery. Sufficient aneurysm occlusion was obtained (B, black arrowhead). During embolization, continuous intra-arterial infusion of Nimodipine was used to reverse vasospasm of the ACA. Furthermore, balloon angioplasty was then performed with the SMB from A1 to A4 segments (C, white arrow). Navigation of the balloon in the distal segments was successfully done by using a 0.007- inch hybrid micro guidewire (Balt Extrusion, Montmorency, France). SAH, subarachnoid hemorrhage; ACA, anterior cerebral artery.
A 56-year-old female (case 3) presented with aneurysmal SAH (Hunt and Hess grade V) and was treated on the 4th post-bleed day for a wide-neck aneurysm (A) of the left posterior inferior cerebellar artery (PICA). A Scepter Mini balloon (SMB) (B, white arrowheads) was used for the balloon remodeling technique due to the morphology of the aneurysm. Catheterization of PICA was performed from the contralateral VA. Navigation of the SMB through tortuous anatomy was achieved with no complication, and occlusion of the aneurysm was obtained (C, black arrowhead). SAH, subarachnoid hemorrhage; VA, vertebral artery.
DISCUSSION
The SMB is an extra-small dual lumen balloon catheter released by MicroVention (Aliso Viejo, CA, USA). Dual lumen balloon catheters are a particular type of catheter with 2 lumina: 1 lumen for balloon inflation, and 1 lumen for injection of liquid embolic agents. They have emerged as an adjuvant tool in liquid embolization. The catheter is placed in an artery supplying the lesion, and embolization is performed after inflating the balloon, which improves distal penetration and prevents reflux of the embolic agent. The safety and efficacy of the Scepter C and XC dual lumen catheters have been previously demonstrated for cAVMs and dAVFs [6,7]. However, the larger caliber (distal outer diameter 2.6 Fr, balloon diameter up to 6 mm) and increased stiffness of their distal portion can make navigation through small, tortuous arterial branches more difficult. Additionally, positioning the catheter tip as close to the target lesion increases both embolization efficacy and safety. With a 1.6 Fr distal tip, a balloon diameter of 2.2 mm, and guidewire compatibility of 0.008-inch or smaller, the SMB provides enhanced navigability with more distal feeding artery access and improves the endovascular treatment of cranial and spinal vascular malformations.
Due to its relatively recent release, the SMB has been mainly reported in scarce case reports and series, mostly involving patients treated with AVM embolization, while only a few articles report data regarding its use in the treatment of intracranial aneurysms. In the first case, the available literature suggests that the catheters perform well with a high degree of technical success [8,9]. A study also supports its use for distal AVF in tortuous and small arterial feeders, especially in the pediatric population, where vessel diameters may be as small as 0.65 mm [10]. The versatility of the catheter and its different applications are also reported in another study, indicating 4 distinct uses: AVF embolization, balloon-occlusion with simultaneous embolization via a second microcatheter, diagnostic angiography with simultaneous balloon obstruction for flow control, and navigation support [5].
The SMB was used in balloon-assisted coiling of distal intracranial aneurysms due to the small diameter or when there was an acute angulation of the parent artery. In summary, 3 of our patients had very small (less than 3 mm) distally-located ruptured aneurysms. Endovascular procedures in small aneurysms have an increased incidence of intraoperative rupture [11]; therefore, we used balloon-assisted coiling to increase the safety of our procedures [12]. Additionally, we used the balloon remodeling technique to avoid the risk of coil protrusion and to achieve complete aneurysmal occlusion in aneurysms with an unfavorable dome-to-neck ratio, while avoiding regrowth or recanalization. In the patient with the PICA aneurysm, the navigability of the SMB allowed us to navigate the microcatheter from the contralateral vertebral across this small diameter parent artery and at the aneurysm neck. Overinflation of the balloon was possible, and coiling was achieved smoothly without complications. The use of the device for combined aneurysm neck remodeling and Woven EndoBridge (WEB; MicroVention) device deployment has also been reported in patients with a small diameter of the aneurysm’s parent artery [13]. The authors of the same study also report a case with a PICA aneurysm treated with SMB, similar to the case we report in our study.
The technique of distal balloon angioplasty has been made known lately [14] as an alternative to the conventional approach (proximal vessel angioplasty and vasodilator infusion for the distal part of the vessel) in patients with postSAH vasospasm. Recent data suggest that the technique substantially reduces the rate of delayed cerebral infarction and recurrence of vasospasm following angioplasty compared to the conventional approach [15]. In 2 of the included cases, the SMB was used for angioplasty of distal branches of the anterior (A4 segment) and middle (M3 segment) cerebral artery. The SMB was more navigable when compared to prior balloons, and no intermediate catheter was used. It is worth mentioning that a 0.007-inch micro guidewire (Balt Extrusion) was used, and distal access was achieved without catheter-induced vasospasm.
CONCLUSION
Based on our experience, the SMB, due to its unique characteristics, could be a safe and efficient device for balloon remodeling of wide-neck ruptured aneurysms of small vessels and distal balloon angioplasty.
Notes
Fund
None.
Ethics Statement
Written informed consent was obtained from the patients, regarding the use of their personal data for scientific and research publication purposes. The study was approved by the Institutional Review Board.
Conflicts of Interest
The authors have no conflicts to disclose.
Author Contributions
Concept and design: II and AA. Data collection: II. Writing the article: II, AA, and NN. Critical revision of the article: NP and MV. Final approval of the article: NP and II. Overall responsibility: AA and II.