Initial Experience Using the New pHLO 0.072-inch Large-Bore Catheter for Direct Aspiration Thrombectomy in Acute Ischemic Stroke
Article information
Abstract
Purpose
A direct aspiration, first pass technique (ADAPT) has been introduced as a rapid and safe thrombectomy strategy in patients with intracranial large vessel occlusion (LVO). The aim of the study is to determine the technical feasibility, safety, and functional outcome of ADAPT using the newly released large bore pHLO 0.072-inch aspiration catheter (AC; Phenox).
Materials and Methods
We performed a retrospective analysis of data collected prospectively (October 2019–November 2021) from 2 comprehensive stroke centers. Accessibility of the thrombus, vascular recanalization, time to recanalization, and procedure-related complications were evaluated. National Institutes of Health stroke scale scores at presentation and discharge and the modified Rankin scale (mRS) score at 90 days post-procedure were recorded.
Results
Twenty-five patients (14 female, 11 male) with occlusions of the anterior circulation were treated. In 84% of cases, ADAPT led to successful recanalization with a median procedure time of 28 minutes. In the remaining cases, successful recanalization required (to a total of 96%; modified thrombolysis in cerebral infarction score 2b/3) the use of stent retrievers. No AC-related complications were reported. Other complications included distal migration of the thrombus, requiring a stent-retriever, and symptomatic PH2 hemorrhage in 16% and 4%, respectively. After 3 months, 52% of the patients had mRS scores of 0–2 with an overall mortality rate of 20%.
Conclusion
Results from our retrospective case series revealed that thrombectomy of LVOs with pHLO AC is safe and effective in cases of large-vessel ischemic stroke. Rates of complete or near-complete recanalization after the first pass with this method might be used as a new benchmark in future trials.
INTRODUCTION
Endovascular thrombectomy has become part of the standard treatment for patients with acute ischemic stroke due to large vessel occlusion (LVO) in the anterior circulation [1,2].
A direct aspiration, first pass technique (ADAPT) has been proposed as a versatile, fast, and cost-effective approach to thrombectomy for acute ischemic stroke, with good recanalization rates and comparatively short procedure times and low associated costs [3,4]. This technique utilizes aspiration as the first approach to revascularize the occluded vessel, and if this strategy fails, then the aspiration catheter (AC) is used in conjunction with a stent retriever to obtain revascularization. Results from numerous single-center reports suggest that the aspiration approach may be less traumatic with minimal vessel wall damage and fewer symptomatic hemorrhages [3,4]. While the Contact Aspiration versus Stent Retriever for Successful Revascularization (ASTER) trial failed to confirm the superiority of this procedure with respect to safety [5], results from the COMPASS trial [4] revealed noninferiority of ADAPT as a first-line procedure for thrombectomy in acute ischemic stroke specifically with respect to functional outcomes achieved when compared to stent retrievers as the first-line approach [5,6].
The current study presents the combined results from 2 comprehensive stroke centers in which patients diagnosed with LVO of the anterior circulation underwent thrombectomies using ADAPT as a first-line approach with the pHLO 0.072-inch large-bore ACs (Phenox), a new larger bore AC that aims to maximize the inner diameter, which has recently emerged and is currently available for use [7,8].
MATERIALS AND METHODS
Endovascular Procedure
The interventional procedures were performed under general anesthesia or conscious sedation, depending on the local setting. An 8F guide sheath (NeuronMAX 0.088 inch; Penumbra or CEREBASE DA 0.090 inch; Cerenovus) was inserted via a transfemoral approach into the internal carotid artery on the affected side. The guide catheter was placed in a distal location (e.g., in the petrous segment if possible).
ADAPT was then performed. The pHLO AC was advanced to the level of the occlusion, typically via a Headway 0.021 (MicroVention) or 0.025 Velocity microcatheter (Penumbra) and a 0.014-inch microwire. A 125-cm pHLO AC was used in 15 of 25 cases (60%); a 135-cm pHLO AC was used in the remaining 10 cases (40%). The procedure was performed using various microwires, including Traxcess 0.014 (MicroVention) and Synchro 2 Support 0.014 (Stryker).
After positioning the pHLO AC with the tip inside the proximal part of the thrombus, the microcatheter and microwire were removed and aspiration was initiated using a vacuum pump. Aspiration was continued for approximately 4 minutes after flow had ceased. The catheter was then removed slowly with additional manual aspiration applied to the guide catheter. If insufficient angiographic recanalization was achieved the aspiration attempt was repeated to engage the clot at the distal tip of the AC; alternatively, an additional thrombectomy device was introduced. The choice between these 2 options was at the discretion of the operator.
Study Design
Approval from the ethics committee of the A.O.R.N. Antonio Cardarelli Hospital was obtained. We retrospectively reviewed all consecutive cases in which ADAPT was performed using the pHLO AC in cases of acute thrombotic strokes at 2 comprehensive stroke centers (October 2019–November 2021). The use of the pHLO AC for endovascular recanalization procedures was at the operator’s discretion at both centers.
Inclusion criteria for endovascular therapy included LVO of anterior circulation as indicated by computed tomography (CT) angiography without evidence of major infarction (Alberta stroke program early CT score ≥6) on either CT or magnetic resonance imaging and a baseline National Institutes of Health stroke scale (NIHSS) score ≥6. All eligible patients received intravenous thrombolytic therapy (IVT), in the absence of contraindications to thrombolytic therapy, as evidenced by the American Guidelines [2] for the early management of acute ischemic stroke patients, a decision taken in any case in mutual agreement with the neurological team.
Procedural and Angiographic Data
Routine demographic data were collected from the patient records. The following parameters were documented from the angiographic images: site of occlusion, accessibility of the clot to the large-bore catheter, final modified thrombolysis in cerebral infarction score (mTICI, with recanalization success defined as a score ≥2b at the relevant site), recanalization success in response to aspiration alone, the need for multiple passages to achieve recanalization, and the need for additional devices. Other parameters recorded included the time elapsed between onset of symptoms and groin puncture (for the first angiographic procedure) and between groin puncture and recanalization, procedure, or catheter-related complications (e.g., vessel dissection), peri-procedural hemorrhage due to vessel perforation, and emboli to distal arteries (EDTs) or new territories (ENTs).
Evaluation of Outcome Data
NIHSS scores on admission and at discharge and the modified Rankin scale (mRS) score at 90 days post-procedure were assessed to identify any post-procedural neurologic deficits. The mRS score was obtained as part of a telephone follow-up or an outpatient visit to a neurologist who was not involved in the initial treatment plan. Favorable clinical outcomes were defined as mRS scores of 0–2.
Follow-up CT scans were obtained 24 hours after treatment in all patients or earlier in cases of clinical deterioration. Intracranial hemorrhage was defined according to the Heidelberg classification.
Statistics
Categorical variables were reported as proportions. Continuous variables were reported as mean±standard deviation or median with interquartile range (IQRs), as appropriate based on the data distribution. In each group, categorical variables were compared using the chi-squared test, and continuous variables were compared using the Kruskal–Wallis test. All statistical analyses were performed using the Stata 14 statistical software package (StataCorp.).
RESULTS
Twenty-five patients who presented with acute stroke between October 2019 and November 2021 underwent endovascular procedures using the pHLO AC. Fourteen patients were female (56%) and 11 were male (44%) with a median age of 71.5 years (IQR, 52–87 years; Table 1). Sixty-eight percent of the patients received IVT. All target lesions were in the anterior circulation (internal carotid artery terminus, n=11; M1 segment, n=14). The time of symptom onset was unknown in 3 of the patients (12%). In all other patients, the median time from the onset of symptoms to the first diagnostic angiogram was 209 minutes (IQR, 120–360 minutes). No tandem occlusions were identified.
Evaluation of Angiographic Data
Successful recanalization was achieved in 24 of the 25 patients evaluated (96%). Post-procedural angiographic results revealed mTICI scores of 2b, 2c, or 3 in 4 (16%), 1 (4%), and 19 (76%) patients, respectively, after multiple maneuvers (IQR, 1–3). Only 1 patient experienced unsuccessful reperfusion (mTICI 2a) after multiple attempts.
The large-bore AC was navigated without the assistance of a stent retriever at the occlusion site in 24 of the 25 cases (96%). Navigation of the AC to the thrombus was not possible in 1 case (4%) due to unsuccessful passage through the origin of the ophthalmic artery. In this case, a stent-retriever (Embotrap III 6x45; Cerenovus) was used to anchor and advance the pHLO AC (Fig. 1A–H). Additional navigation beyond the occlusion site was required in 15 cases (60%); this was successfully provided by a microwire/microcatheter.
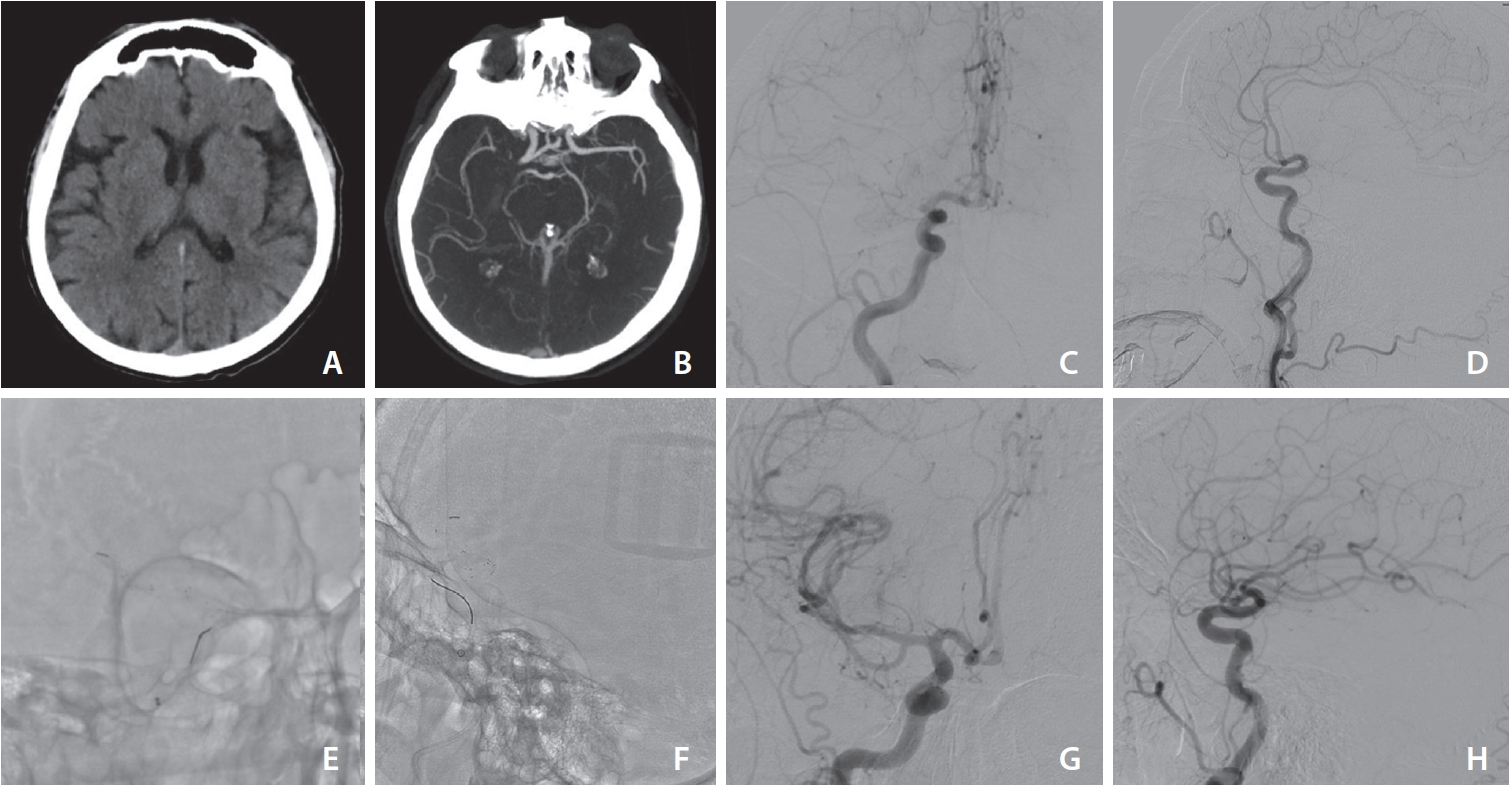
Septuagenarian with a National Institutes of Health stroke scale score of 15, Alberta stroke program early computed tomography score 10 (A), and a right M1 occlusion in computed tomography angiography (B). Digital subtraction angiography in anteroposterior (C) and lateral view (D) confirmed the M1 occlusion with good leptomeningeal collateral circulation. (E, F) Navigation of the pHLO to the thrombus was not possible due to unsuccessful passage through the origin of the ophthalmic artery, so a stent-retriever (Embotrap III 6x45; Cerenovus) was used to anchor and advance the pHLO aspiration catheter. (G, H) Thrombolysis in cerebral infarction score 3 after combined technique. After 3 months the patient’s modified Rankin scale score was 1.
Aspiration alone led to successful outcomes in most patients (19 of 25 [76%]). (Fig. 2A–G) After a first pass, 6 (24%), 3 (12%), and 10 patients (40%) achieved mTICI scores of 2b, 2c, and 3, respectively, with a median recanalization time of 21 min (IQR, 16–30 minutes). After a second pass, 2 additional patients achieved mTICI scores of 3. Thus, we ultimately achieved successful recanalization of the anterior circulation lesions in 21 of the 25 patients (84%) without the need for additional devices.
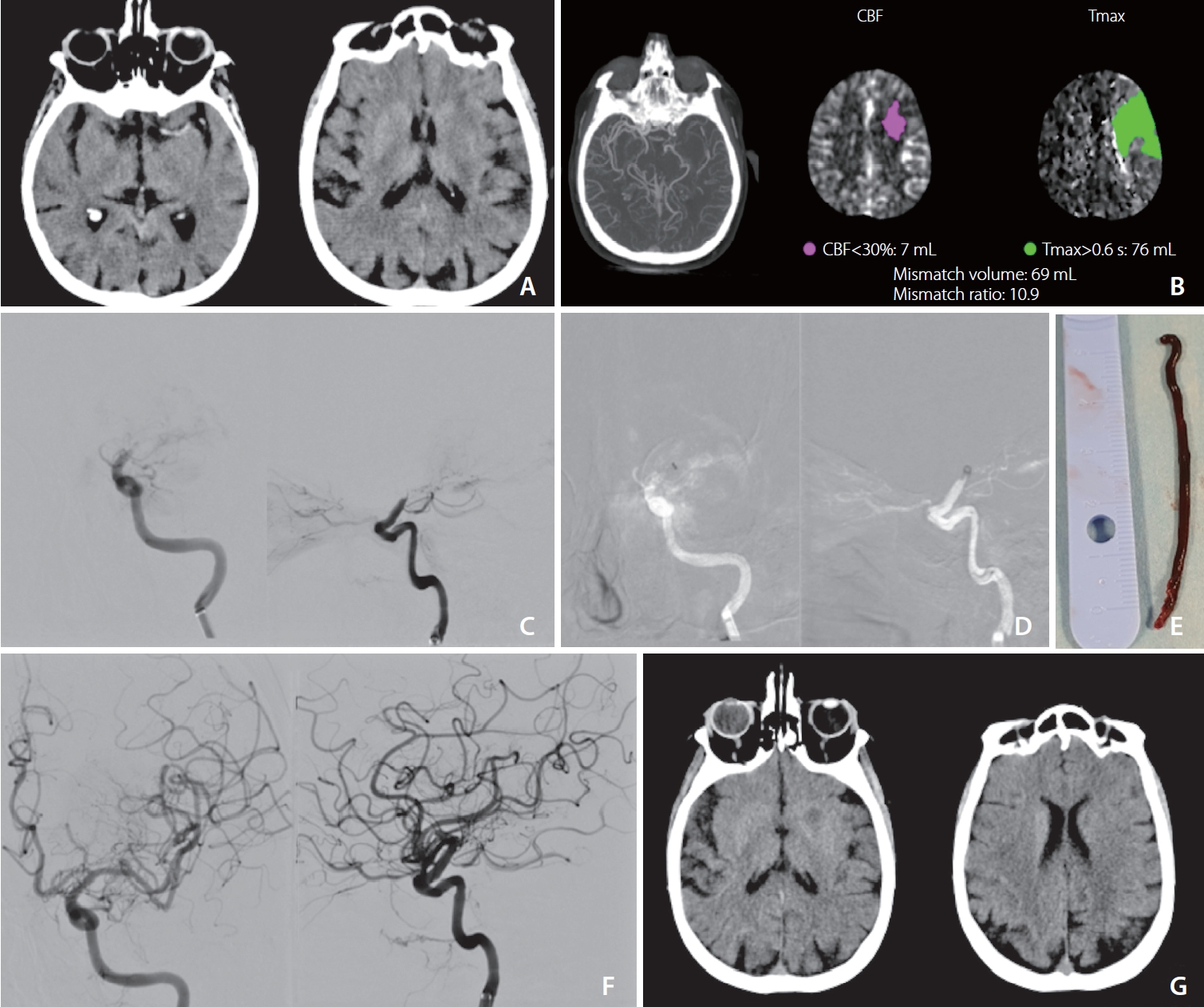
Septuagenarian with a National Institutes of Health stroke scale score of 20. (A) Computed tomography (CT) showed Alberta stroke program early CT score (ASPECT) 7, spontaneous hyperdensity of the left siphon apex extended to the entire M1-M2 tract of the left middle cerebral artery (MCA) (large clot burden). (B) CT angiography confirmed “L” siphon occlusion extended to M1-M2 of the left MCA while perfusion CT angiography obtained by RAPID automated processing showed good mismatch. (C) Digital subtraction angiography confirmed the “L” siphon occlusion (anteroposterior and lateral view). (D) Position of the pHLO at the left siphon apex (anteroposterior and lateral view). (E) Very large entire red clot recovered at first pass. (F) Modified thrombolysis in cerebral infarction score 3 obtained within a procedure time of 18 minutes, anteroposterior and lateral view. (G) CT scan at 24 hours confirmed ASPECT 7. After 3 months the patient’s modified Rankin scale score was 1.
Rescue stent-retriever was necessary for 4 patients (16%, Fig. 1). Three of these patients (12% of the total) ultimately achieved successful recanalization (mTICI 3) with a median recanalization time of 53 min (IQR, 40–67 minutes). Finally, successful recanalization was achieved after multiple passages (maximum of three) in 24 of the 25 cases (96%, Fig. 2).
Evaluation of Outcome Data
The median NIHSS score at presentation was 16 (IQR, 6–24). At discharge, the median NIHSS score of the patients who survived for an additional 3 months or more was 7.7 (IQR, 0–23). Five of the patients (20%) died within 3 months of undergoing the procedure (2 fatal pneumonias, 1 sepsis, 2 fatal myocardial infarctions), mRS scores of 0–2 were achieved in 13 of the 25 patients (52%).
There were no statistically significant differences in the outcomes between patients who received IVT and those who did not receive IVT.
Complications
Four patients developed EDTs during the procedure performed with the pHLO AC. In 2 of these cases (8%), a stent retriever was required. No ENTs were detected. CT studies performed 24 hours post-procedure revealed no hemorrhagic transformation in 17/25 patients (68%). While 4 (16%) and 3 (12%) of the patients exhibited hemorrhages scored at hemorrhagic infarction type 1 and 2 (HI1 and HI2), respectively, only 1 patient (4%) developed symptomatic parenchymatous hematoma type 2 (PH2), according to Heidelberg bleeding classification. No perforation, dissections, or other complications were reported.
DISCUSSION
The revascularization rates observed in our patient series are consistent with and in some cases superior to those reported in the literature [7-17]. In this study, we successfully recanalized 76% of the anterior circulation thrombi at the first pass. This fraction grew to 96% when using a combination of techniques. Functional independence, as well as the rates of mortality and the development of symptomatic intracranial hemorrhage, were similar to those reported in the aforementioned recent meta-analysis [17]. In other retrospective case series, 25% of the cases that featured a large-bore AC required the concomitant use of a stent retriever; the latter device functioned as an anchor that delivered the AC up to the level of the thrombus [8,17-21]. In our study, the thrombus site was accessible to the large-bore AC in most of the cases (96%) and did not require support from a stent retriever.
No ENTs were reported in our patient series, and the frequency of EDTs requiring a stent-retriever (at 8%) was similar to that reported in recent literature [22] on stent-retriever or combined techniques. EDT rates varied in different case series, largely reflecting variations in the location of the target occlusion, the composition of the thrombus, whether or not IVT was provided to patients before endovascular treatment, and the types of thrombectomy devices used [23,24].
Our results find numerous confirmations in the literature. Li and Ribo [25] reviewed the clinical experience and in vitro studies of REACT ACs (Medtronic), large-bore ACs that feature a polytetrafluoroethylene liner, and nitinol reinforcement. In vitro studies support the effectiveness of REACT catheters. The rates of procedural success and recanalization at the first attempt, along with the null incidence of complications related to REACT catheters, demonstrate the safety and effectiveness of the devices, in terms of clinical experience [25]. Another recent study [26] reported initial experience in 9 patients with AXS Vecta 71 and 74 for mechanical thrombectomy using aspiration and combination techniques for the purpose of assessing their safety and efficacy, resulting in successful revascularization in a similar proportion of cases as previously published studies (89%), using both ADAPT and the stent-retriever plus a local aspiration technique, without complications.
A recent meta-analysis [14] including 20 studies with a total of 6,311 patients revealed that ADAPT resulted in similar clinical outcomes compared to procedures performed with stent retrievers, albeit requiring more likely additional therapy compared to those in the stent retriever group. Results from previous studies reveal that anatomical and technical factors have a significant influence on the likelihood of effective recanalization. From an anatomical point of view, the site of arterial occlusion [2] and the angle of interaction between the thrombus and the AC [15] were both associated with the likelihood of successful recanalization.
The ACs used in these procedures must be trackable so that they can be navigated easily and atraumatically through tortuous intracranial vessels. Some concerns were raised regarding the safety of navigation using these large bore devices, especially when used in procedures involving tortuous vessels at the ophthalmic artery. These catheters must also have a large inner diameter and wall strength that will accommodate maximum aspiration force and resist collapse. To address this concern, the ACs are typically constructed in multiple segments of varying flexibility with those that are stiffer in proximal locations and those that are more compliant distally [16].
This latter principle was highlighted in a recent study of the physical properties of ACs used in thrombectomies performed on stroke patients that focused on catheter tip force, aspiration flow rates, and effective flow lumens [15]. As shown, larger internal diameters will result in lower resistance (R) and a larger flow rate (Q). As shown, larger inner lumen diameters are more effective at promoting thrombus removal [15]. While these properties have not yet been explored in large clinical trials [4,5], the results of this analysis might explain the higher efficacy profiles of procedures involving ADAPT. For example, results from a recent meta-analysis published by Gory et al. [17] reported successful recanalization (i.e., mTICI scores of 2b–3) using ADAPT in 66% of cases of acute stroke; a rescue strategy using a stent retriever in another 31% of the cases yielded an overall 89% success rate at achieving mTICI scores of 2b–3.
Our study has several limitations. We recognize the limitations inherent in its design, the number of enrolled patients in 2 centers, and the absence of a control group. Furthermore, the angiographic images were assessed by the interventional neuroradiologist performing the endovascular procedure and thus might be biased toward higher mTICI scores.
CONCLUSION
Results from our retrospective case series revealed that thrombectomy of LVOs performed using ADAPT with a large-bore pHLO AC is safe and effective in cases of large-vessel ischemic stroke. Our findings revealed no complications that were directly related to AC positioning. Other complications, including EDT and intracranial hemorrhage, occurred with frequencies that are consistent with earlier reported procedures that used other ACs [2-8].
Notes
Fund
None.
Ethics Statement
Approval from the ethics committee of the A.O.R.N. Antonio Cardarelli Hospital was obtained. We anonymized the patient informations that may identify the patients.
Conflicts of Interest
The authors have no conflicts to disclose.
Author Contributions
Concept and design: GL. Analysis and interpretation: GL, Massimo Muto, GG, PC, GS, ES, and ADM. Data collection: GL, Massimo Muto, FG, ADD, CR, DGR, PC, ES, and ADM. Writing the article: GL, CR. Critical revision of the article: GL and VA. Final approval of the article: FG, CR, GS, VA, and Massimo Muto. Statistical analysis: FG, CR, DGR, ES, and Massimo Muto. Overall responsibility: GL and Mario Muto.

