Off-Label Application of Pipeline Embolization Device for Intracranial Aneurysms
Article information
Abstract
Purpose
The Pipeline embolization device (PED) is approved in the USA for treating giant and large aneurysms arising from the petrous to superior hypophyseal segments of the internal carotid artery in patients older than 21 years of age. This study investigates off-label PED results in a large cohort.
Materials and Methods
Retrospective, single-center review of all patients who had off-label PED surgery.
Results
Sixty-two aneurysms (48 patients) underwent off-label PED treatment from 2012–2017. There were 44 females and four males (age 21 to 75 years; mean/median, 54.3/55.0 years). The most common presenting symptom was headache (47/62, 75.8%). All aneurysms were in the anterior circulation. Aneurysm size ranged from 1.4 to 25.0 mm (mean/median, 7.6/6.9 mm). Fifty-two aneurysms had post-operative imaging with total/near-complete occlusion of 84.6% (44/52). Aneurysm-based operative near-term complication rate was 9.7% while there were no permanent complications. For aneurysms and headache, 86.7% improved/resolved after embo-surgery, and were four times more likely to have a better clinical outcome (resolved or improved symptoms) after surgery (odds ratio [OR], 4.333; P=0.0325). Left-sided aneurysms had a higher occlusion rate (OR, 20; P=0.0073). Hypertension (OR, 4.2; P=0.0332) and smoking (OR, 7; P=0.0155) were more prone towards aneurysm occlusion. Patients without a family history were 14 times more likely to have favorable imaging outcome (P=0.0405). There is no difference of occlusion rates between untreated and previously treated aneurysms (P=0.6894). Overall, occlusion rate decreased by 14% with an increase of aneurysm size by 1 mm (P=0.0283).
Conclusion
For anterior circulation aneurysms, the off-label application of PED is as effective and safe as reported for on-label intracranial aneurysms.
INTRODUCTION
In 2011, the U.S. Food and Drug Administration approved Pipeline embolization device (PED) as the single flow divertor [1] for the use of treatment in large or giant wide-necked internal carotid artery aneurysms from the petrous to the superior hypophyseal segments in patients who are 22 years of age or older [2]. Ever since, the application of PED has been explored in multiple off-label scenarios [3]. However, the value of PED in treating aneurysms outside of the aforementioned criteria such as those that are <10 mm in diameter, distal to superior hypophyseal artery, fusiform/tandem/blood blister-like in shape, previously ruptured/treated, etc., remains unclear. Our study aims to elucidate the off-label role PED plays in treating these aneurysms.
MATERIALS AND METHODS
This study is a single-institute retrospective study investigating patients who underwent off-label PED treatment between January 1, 2012 and December 30, 2017. The study was Institutional Review Board (IRB) of Baylor Scott & White Health approved and consent was waived due to the retrospective, observational nature of the study (IRB 017292).
Inclusion criteria
On-label PED indications are: age ≥22 years; size ≥10 mm; neck ≥4 mm or dome/neck <2; aneurysm location from petrous to superior hypophyseal internal carotid artery. Treated aneurysms that did not fit these criteria were considered as off-label and were enrolled. Typical examples included: aneurysm size <10 mm; previously ruptured aneurysms with recurrence that were coiled/stented or clipped; tandem/blood blister-like/fusiform aneurysms; aneurysms distal to superior hypophyseal artery.
Peri-operative anti-platelet management
All elective cases were treated with dual anti-platelet therapy (DAPT) before the deployment of PED with either aspirin (81 mg daily or 325 mg daily) and clopidogrel (75 mg daily), or aspirin (81 mg daily or 325 mg daily) and ticagrelor (90 mg twice a day, used for clopidogrel hypo- or non-responders) for 7–10 days prior to procedure. For emergent cases, a loading dose of aspirin (650 mg) and clopidogrel (375 mg) was used. P2Y12 platelet response tests for clopidogrel and aspirin were not routinely obtained as this lab analysis regimen varied both among surgeons and even varied with individual surgeon during the study period. However, for clopidogrel non-responders, ticagrelor was utilized. There was one case where eptifibatide drip was administered intra-operatively. For all patients, aspirin was maintained up to 1 year, while the other anti-platelet medication was continued for at least 3 to 6 months.
Follow-up assessment
The endpoint was either radiographic evidence of occlusion or patient’s last clinical assessment. Computed tomography angiography (CTA), magnetic resonance angiography (MRA), and digital subtraction angiography (DSA) were used for the evaluation of occlusion. The results were classified as complete occlusion (100%), near-complete occlusion (90–100%), incomplete occlusion (<90%), or no effect (0%). Routine screening in asymptomatic patients for complications such as ischemic/hemorrhagic strokes was not performed. Clinical notes by either Neurosurgery or other specialties such as Neurology, Family Medicine, were checked for baseline and post-operative, aneurysm-related symptoms. Clinical outcomes were classified as 1) improved/resolved, 2) persistent/unchanged, 3) asymptomatic both pre- and post-PED, and 4) new symptoms.
Statistical analysis
Univariate logistic regression models were implemented to select the possible predictors. A P-value of less than 0.2 was included as possible predictors in the final model. A multivariate logistic regression model was fit to the data. The Hosmer-Lemeshow test was used to assess fitness of data. Candidate predictors were variables that had P-values of 0.2 or less. These variables were: headache, side, smoking, family history, and size. All of the potential predictors were included in the final model. The forward and backward model selection procedures were used to find the potential predictors. Therefore, the binary clinical outcome (improved and resolved versus other clinical outcomes) and image results were evaluated by multivariate logistic regression, adjusted for side, smoking, family history, and size. All the P-values were reported. The c-statistics were equal to 0.86 and 0.77 for clinical outcome and image results separately, indicating that the models predict about 86% and 77% of the variability in the model. The Hosmer-Lemeshow test indicates a good fit to the data. A P-value of less than 0.05 was considered as significant. All statistical analysis was performed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
A total of 62 aneurysms underwent off-label PED treatment during the study period, and these were enrolled for data analysis (Table 1). A total of 54 procedures were performed. All of these aneurysms were treated by surgeons: W.L. (48), E.B. (6), and others (8).
Demographic characteristics
The 62 aneurysms afflicted 48 total patients (44 females and four males). Age range was 21 to 75 years of age with a mean age of 54.3 years and median of 55.0 years. Forty-one aneurysms were in Caucasian patients, eleven in African descent patients, six in Hispanic patients, three in Asian patients, and one in a Puerto Rican patient. The most common presenting symptom was headache (47/62, 75.8%). Other symptoms included cranial nerve-III deficits (5, 8.1%), vision changes (9, 14.5%), dizziness/vertigo (7, 11.3%), tinnitus (5, 8.1%), nausea/vomiting (3, 4.8%), and dysphasia (1, 1.6%). Ten aneurysms were discovered in asymptomatic patients. The most common co-morbidities included hypertension (41, 66.1%) and diabetes mellitus (4, 6.45%). Five (8.1%) aneurysms were in patients with a family history of cerebral aneurysm, and 46 (74.2%) aneurysms were in patients with a positive smoking history.
Aneurysm characteristics
The size of the aneurysms ranged from 1.4 mm to 25.0 mm, with a mean of 7.6 mm and median of 6.9 mm. The neck size ranged from 1.2 mm to 12 mm with a mean of 4.2 mm and a median of 3.9 mm. Forty-five (72.6%) aneurysms were small aneurysms (largest diameter <10 mm). Thirty-two (51.6%) aneurysms were on the left side and 30 (48.4%) aneurysms were on the right side. The specific locations of the aneurysms were distributed as following: ophthalmic (12, 19.4%), posterior communicating (12, 19.4%), supra-clinoid (11, 17.7%), superior hypophyseal (8, 12.9%), cavernous (6, 9.7%), para-clinoid (6, 9.7%), dural ring (6, 9.7%), and M1 (1, 1.6%). The shapes of the aneurysms were classified into the following five groups: saccular (46, 74.2%), lobulated (8, 12.9%), tandem (3, 4.8%), blood blister-like aneurysm (3, 4.8%), and fusiform (2, 3.2%). Fourteen aneurysms were ruptured (22.6%). Due to the multiple treatment combinations, pre-PED interventions were comprised of nineteen (30.7%) endovascular and four (6.45%) open surgeries in twenty aneurysms (32.3%): twelve (19.4%) underwent coiling only; two (3.2%) underwent stenting only; two (3.2%) underwent coiling and stenting; two (3.2%) underwent coiling, stenting, and clipping; one (1.6%) underwent clipping only; one (1.6%) underwent both coiling and clipping.
Treatment and post-operative course
Pre-operatively, all aneurysms received aspirin therapy. Sixty-one (98.4%) aneurysms received clopidogrel, two non-responders and the remaining one received ticagrelor (4.8%). Sixty (96.8%) aneurysms were treated by PED only and two (3.2%) aneurysms were treated with PED and coiling. Post-operatively, all aneurysms continued with aspirin. All but four aneurysms were managed with aspirin and clopidogrel regimen. In the four (6.5%) that received variation of DAPT, three were treated with ticagrelor, while the fourth aneurysm developed intra-operative PED platelet aggregation prompting eptifibatide drip which was later switched to oral aspirin and clopidogrel therapy. All aneurysms were treated with a single PED. Two (3.2%) aneurysms received adjunctive coil embolization. Out of the 14 ruptured aneurysms, only one received emergent PED on post-bleeding day (PBD) 3 which appeared to be blood-blister like on DSA on PBD 1. She was loaded with 650 mg Aspirin and 180 mg Ticagrelor (Clopidogrel non-responder) on the day before the PED embolization. All other 13 were treated as an elective case based on follow-up imaging indicating non-occlusion (ranges from 1 month to 100 months; mean, 24 months; median, 10 months). Aneurysm-based complication rate was 9.7% (6/62), including one patient who had two aneurysms (Table 2). When calculated as procedure-based, the complication rate dropped slightly to 9.3% (5/54). However, all patients’ complications quickly resolved, and they were discharged without permanent neurological deficit. The length of stay ranged from 1 night (48, 77.4%), 2 nights (10, 16.1%), 3 nights (2, 3.2%), 5 nights (1, 1.6%), and 21 nights (1, 1.6%). The prolonged 21 nights stay was for a patient presenting with a ruptured blood blister aneurysm.
Follow-up
Fifty-two (83.9%) aneurysms had post-operative imaging at an average follow-up of 327 days and a median of 358 days. Most aneurysms received initial radiographic evaluation between 6 months and 1 year post-operatively. MRA was the most commonly used method for 31 aneurysms (59.6%), while DSA was obtained for 17 aneurysms (32.7%) and CTA was utilized in four aneurysms (7.7%). Among the four aneurysms followed with CTA, three aneurysms were in one patient with triplet tandem aneurysms.
The total/near-complete occlusion rate was 84.6% (44/52); partial occlusion was achieved in seven aneurysms (13.5%); and only one aneurysm (1.9%) had no response to PED (Table 3). As seen from Tables 4 and 5, aneurysms on the left side had a higher occlusion rate (odds ratio [OR], 20; P=0.0073). Aneurysms in patients with a history of hypertension (OR, 4.2; P=0.0332), smoking (OR, 7; P=0.0155), and without a family history (OR, 14; P=0.0405) were more likely to respond to PED, separately. With an increase of aneurysm size by 1 mm, the occlusion rate on follow-up imaging decreased by 14% (P=0.0283). As for the 20 aneurysms previously treated with either coiling or clipping or both, 16 have follow-up imaging with an occlusion rate of 81.25% (13/16). Out of the remaining 42 previously untreated aneurysms, 31 out of the 36 that has follow-up imaging achieved total occlusion, resulting a rate of 86.11%. There is no statistical difference for the occlusion rate between two groups (P=0.6894).
Sixty (96.8%) aneurysms had clinical follow up with an average of 383 days and a median of 367 days. Among them, 48 (80.0%) aneurysm-associated symptoms improved/resolved, seven (11.7%) persisted, four (6.7%) asymptomatic aneurysms remained so both pre- and post-PED, and one (1.7%) had new symptom of headache (Table 3). For 45 (72.6%) aneurysms with pre-PED headache, 39 improved/resolved (39/43, 90.7%; two missing follow-up). Overall for aneurysms with associated headaches, following PED treatment, these aneurysms had a four-fold increased likelihood for improved/resolved headaches (OR, 4.333; P=0.0325 by univariate analysis; not significant by multivariate analysis).
DISCUSSION
Gender distribution
In our study, the female to male ratio of 11.4:1 is dramatically skewed from the known aneurysm prevalence of 3:2 distribution. However, similar demographics were also reported in other studies [4,5]. Becske et al. [4] attribute the bias to two factors: 1) gender predilection for the cavernous internal carotid artery [6] and 2) referral bias. Other contributing factors that may explain these results include: 1) females seem to have an increased risk of formation and growth of intracranial aneurysms [7-9] and 2) women more frequently seek medical attention than men [10].
Headache and treatment
Headache is a common presentation of unruptured intracranial aneurysms, with a reported rate of 18–34% [11]. Studies have pointed out that the structural change of the artery that disturbs the innervating nerve could be the mechanism, and that treatment of the aneurysm can be effective in improving the symptoms [12,13]. Kong et al. [14] reported that after clipping or coiling treatment of aneurysms, 89.8% patients’ headaches improved. Our study corroborates this favorable outcome in patients with headaches who undergo PED-based aneurysm surgery. On the other hand, endovascular aneurysm surgery may rarely cause de novo headaches. In our study, there was just one patient with new headache after treatment, accounting for only 1.6% of total aneurysms treated. Others have reported similar low incidence of new post-operative headache, but when it occurs, it tends to resolve over time [15].
Smoking
Our data reveals that patients with a smoking history have a better occlusion rate (OR, 7; P<0.05). Similarly, both Adeeb et al. [16] and Griessenauer et al. [5] found that smoking status had a significantly favorable relationship with the occlusion of the aneurysms. However, by stratifying 694 aneurysms treated with PED into never, current, former smoker groups, Rouchaud et al. [17] could not conclude that smoking affected occlusion rates. Given that smoking has long been identified as a risk factor for the formation, growth, and rupture of intracranial aneurysms [7,8,18-20], further study of smoking history and PED occlusion response is warranted.
Family history
Patients with a family history of aneurysms had a lower occlusion rate to PED (OR, 14; P<0.05). We postulate that different mechanisms of formation and growth of aneurysms in patients with a family history may influence the in vivo response to PED. Studies have shown that inflammation plays an important role in the aneurysms formation and growth in smokers [18] while familial aneurysms may be related to genetic disorders [21]. Further research on these different responses to PED treatment of aneurysms is warranted.
Outcomes of PED treated aneurysms
The occlusion rate of aneurysms has been reported at various follow-up intervals and tends to increase as the follow-up time elongates [22]. Though there is no consensus as to when the imaging follow-up should be performed; in general, 6 months to 1 year is commonly used. Various sources have reported an occlusion rate ranging from 75% to 95% [16,22-24]. Our study has a mean/median follow-up of 327/358 days. The total/near-complete occlusion rate achieved 84.6%. Our data indicates that off-label PED treatment is as effective as on-label application. Among the 45 small aneurysms, 37 (37/45, 82.2%) had follow-up imaging, and 31 (31/37, 83.8%) had complete occlusion, five (5/37, 13.5%) had partial occlusion, only one (1/37, 2.7%) remained no change. In another study of small aneurysms treated with PED, it was reported to have a complete occlusion rate of 72%, and partial occlusion rate of 28% at a mean follow up of 6.3 months [25]. Among the 14 ruptured aneurysms, 11 (11/14, 78.6%) aneurysms had follow-up imaging, and 10 (10/11, 90.9%) of them revealed complete occlusion, including the one treated emergently on PBD 3, while only one (1/11, 9.1%) aneurysm remained no change at post-operative day (POD) 303. Chalouhi et al. [26] reported a similar complete occlusion rate of 80% for ruptured aneurysms treated with PED. For aneurysms with previously failed coiling/clipping therapy, our occlusion rate reached 86.11% after PED embolization which indicates that PED is an excellent backup/rescue option for these aneurysms. We included one case with three tandem aneurysms that were all occluded on POD 219 (Fig. 1). Awad et al. [27] reported PED treatment for tandem aneurysms in seventeen patients with a mean final Raymond-Roy score of 1.3±0.7. We had one unruptured, previously untreated M1 aneurysm that was found during the work-up of tinnitus in a 64-year-old female patient. On POD 406 of PED treatment, it regressed in size but was not occluded on the MRA study. Cagnazzo et al. [28] performed a meta-analysis on middle cerebral artery aneurysms treated with PED and found a complete/near-complete occlusion rate of 78.7%. A recent prospective multicenter trial of flow diversion for small and medium size aneurysms (PREMIER trial) [29] evaluated 144 patients with intracranial aneurysms measuring less than 12 mm, and 84.4% of which were less than 7 mm [30]. Patient characteristics were similar with our study. A single PED was successful in treating 92.9% of all aneurysms. Rate of major stroke or death was 1.4% at 30 days and 2.1% at 1 year. Occlusion rate at 1 year was 83.5%, similar to our results of 84.6%. Although outcomes were similar, the PREMIER trial included aneurysms in the vertebral circulation up to the PICA, which our study only included aneurysms in the anterior circulation (internal carotid and middle cerebral artery).
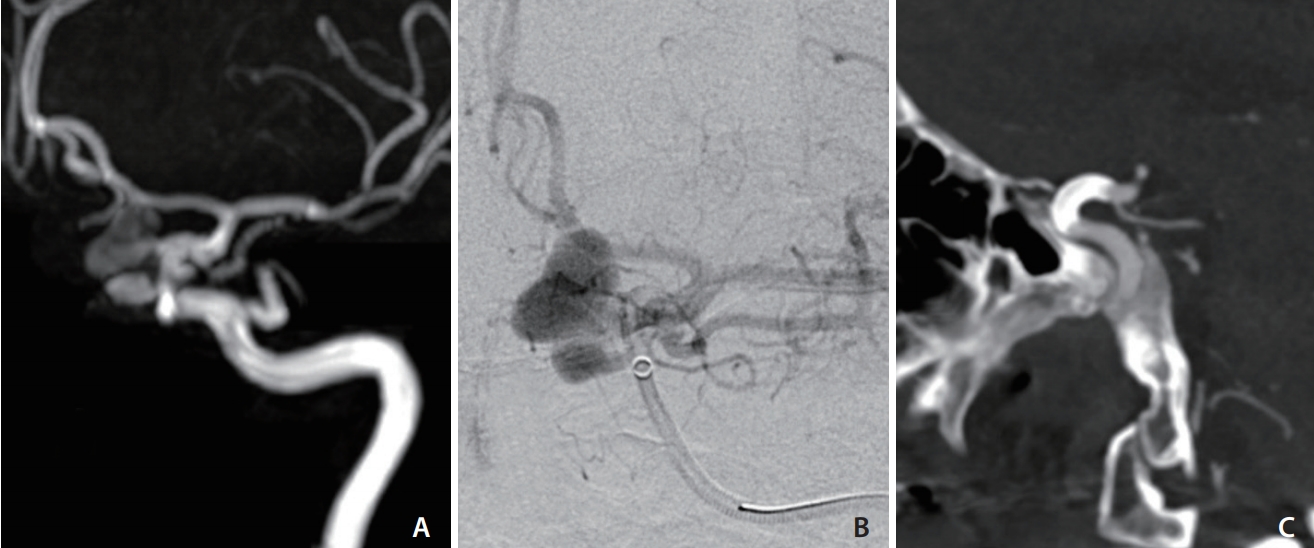
(A) Three aneurysm cluster is seen on MRA imaging before the PED treatment. (B) Digital subtraction angiogram presentation of the triplet aneurysms. (C) Follow up sagittal CTA reveals that all three aneurysms are occluded (post-PED day 219). MRA, magnetic resonance angiography; PED, Pipeline embolization device; CTA, computed tomography angiography.
Left-sidedness
An interesting phenomenon observed in our study is that the aneurysms in the left anterior circulation had a better occlusion rate than those on the right side. Since PED promotes aneurysm regression in part by disruption of blood flow, a baseline difference in blood flow between the right and left carotid arteries might influence occlusion rates with PED. By using Doppler duplex scanner, Ackroyd et al. [31] concluded that there was no significant difference of blood flow between the two carotid arteries in normal people. However, Urbanski et al. [32] inspected the blood flow in the carotid arteries after cannulation and found that even though the flow rates were similar, the perfusion pressure was significantly higher in the left carotid than in the right carotid artery. In this study, higher occlusion rate was observed in both hypertension and in left-sidedness which seems to correlate with the phenomenon report by Urbanski et al. [32] However, Schneiders et al. [33] discovered that a flow diverter seems to have no effect on reducing the pressure in the aneurysm. As shown by previous studies, the mechanism of PED on aneurysms includes both stagnation of the blood flow in the aneurysm, which leads to thrombosis within the aneurysms, and endothelialization/neointima growth over the device strut at the aneurysm neck [34,35]. It is unclear if higher perfusion pressure is related to either one of these mechanisms. ASPIRe [23] study collected data on the sides of the aneurysms but did not mention any related occlusion difference. Several large studies [4,22,36,37] have not reported outcome data regarding side of treated aneurysms. Nevertheless, the laterality of the aneurysm may be a weak or minor variable possibly impacting the flow dynamics of Pipeline flow diversion.
Complications after treatment
Aneurysm rupture, intraparenchymal hemorrhage, and ischemic strokes are the three most severe morbidities among patients treated with PED [23]. The treatment-related morbidity rate has been reported to range from 4% to 10% [28]. In our study, aneurysm-based morbidity was 9.9%, in which all events were short-term, and fully resolved by the time of discharge. In our study, there was no mortality. It is also worthwhile to mention that the patient with ruptured aneurysm loaded with DAPT before PED on PBD 3 recovered well with no new bleeding during the hospital course. This data indicates that off-label PED treatment is as safe as on-label applications.
Limitations
This study is limited by its nature of retrospective design. Due to the number of cases, we did not further subdivide these off-label cases into additional groups for analysis. While we do not have extended-term follow-up of PED cases (>2 years) to exclude recanalization following aneurysm occlusion, all studies to date do not indicate that recanalization occurs after Pipeline treatment.
CONCLUSION
For anterior circulation aneurysms, the off-label application of PED is as effective and safe as reported for on-label intracranial aneurysms.
Acknowledgements
This study was presented in part at the 2018 American Association of Neurological Surgeons Annual Scientific Meeting in New Orleans, Louisiana, USA, April 28–May 2, 2018.




