Physiologic Flow Diversion Coiling Technique for Wide-Necked Aneurysms with an Asymmetric Bidirectional Flow at the Aneurysm Neck
Article information
Abstract
Purpose
Wide-necked aneurysms in the circle of Willis (CoW) are prone to recur due to reciprocal bidirectional flow. We present a novel concept of coil embolization to prevent recurrence that uses physiologic flow diversion at the CoW.
Materials and Methods
We enrolled 14 patients (15 aneurysms) who underwent aneurysm coiling for wide-necked aneurysms with asymmetric bidirectional inflow into the aneurysm. Four patients had recurrent aneurysms after coiling. The concept of physiologic flow diversion included obliterating antegrade flow into the aneurysm sac as well as opposite CoW flow by performing compact coil packing with intentional protrusion out of the aneurysm neck to the communicating part.
Results
Fifteen aneurysms, including 4 recurrent aneurysms, in an anterior communicating artery (n=7), posterior communicating artery (n=5), and tip of the basilar artery (n=3) were treated with coil embolization (n=10) and stent-assisted coiling (n=5). All aneurysms had a wide neck, and the mean largest diameter was 9.0 mm. The mean packing density was 45.1%. Twelve aneurysms were completely occluded, and 3 aneurysms had tiny residual neck remnants. There was neither a neurological event nor recurrence during the mean 12.5 months of follow-up.
Conclusion
Wide-necked aneurysms at the CoW tend to recur. As a strategy to prevent a recurrence, physiologic flow diversion can be an option in treating wide-necked aneurysms in the CoW.
INTRODUCTION
With the in-depth understanding of aneurysm formation and the development of endovascular devices, endovascular treatment for the unruptured intracranial aneurysm and management of a patient with the aneurysm have been advanced recently [1-5].
The circle of Willis (CoW), a basal network of cerebral arteries connecting to the brain circulation, includes the anterior communicating artery (ACoA) and posterior communicating artery (PCoA) as important elements. This junction area in the CoW was found to be the most likely geographic area to harbor the formation of an aneurysm [6]. Blood flow dynamics are considered an important factor in the pathogenesis and treatment of cerebral aneurysms [6,7]. While some studies on cerebral hemodynamics have provided useful information on cerebral aneurysm formations in the CoW, little emphasis has been given to the role of the CoW in aneurysm recurrence [8].
The asymmetry in the CoW raises wall shear stress and may play a critical role in the development and recurrence of cerebral aneurysms after treatment [9-12]. This risk increases with the degree of flow contribution from the 2 adjacent anatomical segments of the CoW. This difference may result from the actual difference in the artery diameters, or it may be due to variation in the blood flow among the carotid and basilar arteries across the ACoA and PCoA. As anterior cerebral artery (ACA) A1 dysplasia/hypoplasia is known to be a potential risk factor in the formation of an ACoA aneurysm, a reciprocal hemodynamic relationship that is dependent on the development of the CoW may also affect aneurysm recanalization after endovascular treatment, especially when there is loose coil packing in the aneurysm compared to the dense packing [13,14]. Other risk factors for recurrence include a large aneurysm size, a thrombosed aneurysm, low packing density (PD), initial incomplete occlusion, a ruptured aneurysm, and a large neck-dome ratio [15].
The main principle of endovascular treatment of intracranial aneurysms includes the achievement of angiographic occlusion and high PD while preserving blood flow in the parent, branching, and perforating vessels [15,16]. Several techniques such as the double microcatheter technique, balloon-assisted coiling, and stent-assisted coiling are currently adopted to follow the principle but require additional devices and related cautions [15]. Although high PD of a coil for the treatment of aneurysms is required to minimize recanalization or risk of rebleeding, it cannot be done without the risk of compromising flow in the CoW, which may cause inadvertent infarction [17].
In this study, we modified the endovascular strategy to occlude the aneurysm as much as possible by allowing partial occlusion of the ACoA or PCoA, which fills from the opposite direction to the aneurysm in the CoW and, thus, induces vessel hypertrophy to overcome the cerebral perfusion and avoids a possible inadvertent hemodynamic compromise. We call this concept physiologic flow diversion, which facilitates reciprocal flow in the CoW to induce hypertrophy of the collateral vessels and leads to reducing recanalization of the aneurysm. We present the outcomes and follow-up results of patients treated by following this technical concept.
MATERIALS AND METHODS
Patient Population
Approval from the institutional review board was obtained (No. 2021-1102). Informed consent was waived for this retrospective study. We retrospectively evaluated the prospectively-collected neurointervention system database for all neurointerventional procedures at our institution from January 2018 to April 2021. In this period, we treated 958 unruptured intracranial aneurysms in 810 patients. We included aneurysms that developed at the junction of the CoW, such as the ACoA, PCoA, and the tip of the basilar artery (basilar tip), and that were treated using the physiologic flow diversion embolization technique. We excluded aneurysms that were located in a part of the CoW, especially when the contralateral side of the vessel was aplastic and that underwent clipping surgery. Fourteen patients who underwent endovascular treatment for aneurysms (n=15) using the physiologic flow diversion embolization technique were included in this study. General characteristics, pre and post modified Rankin Scale (mRS), and follow-up durations were evaluated. Aneurysm characteristics, procedure information (treatment, PD, and outcome), and follow-up magnetic resonance angiography (MRA) were evaluated. Informed consent was obtained from patients who agreed to allow publication of their history and radiological images.
Physiologic Flow Diversion Embolization Technique
If a patient has a wide-necked aneurysm with an asymmetric bidirectional inflow into the aneurysm at the junction of the CoW, such as the ACoA, PCoA, and basilar tip, physiologic flow diversion was applied in the endovascular procedure. The concept of physiologic flow diversion included performing compact coil packing via the dominant flow side and occluding the opposite CoW flow by an intentional protrusion of the coils out of the aneurysm neck to the communicating part. Such over-packing of the coil induces remodeling of the CoW by retrograde flow from the nondominant flow side to induce progressive development of flow in the nondominant flow side during a certain period after embolization (Fig. 1). In the case 2 (patient 9), we planned a sequential embolization. Initially, we densely packed the coils in the aneurysm sac and its communicating segment via the dominant artery (initial closure of the front door). After 2 months, the aneurysm neck of the nondominant side was partially recanalized (opening of the back door) as the nondominant side flow progressively increased to compensate for the distal flow. Additional coiling through the enlarged nondominant artery was applied (secondary closure of the back door; Fig. 2). This, therefore, secured the densely packed coil in the aneurysm neck (closure of back door) without recurrence from the dominant flow side (reopening of the front door).

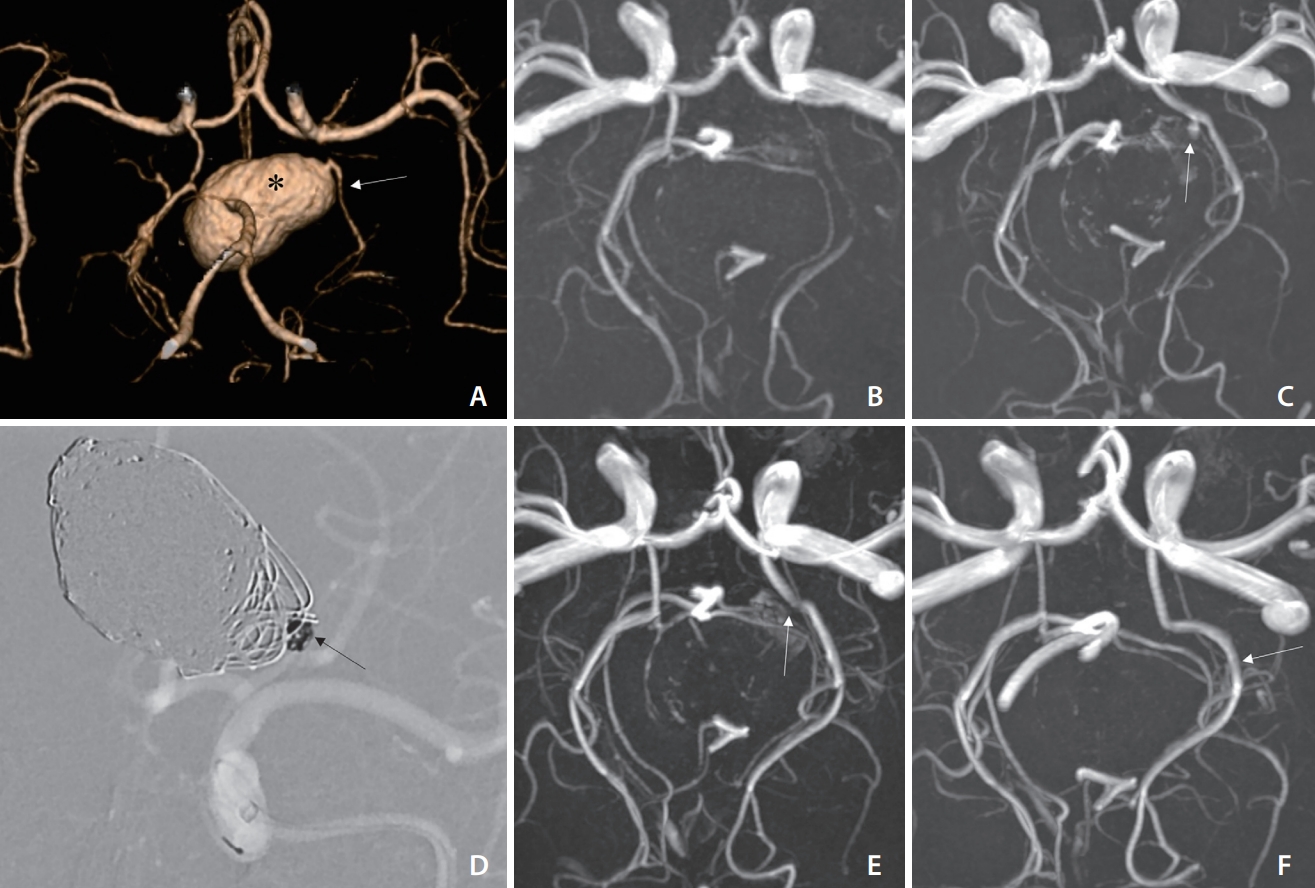
An adult patient (patient 6) with a giant thrombosed anterior communicating artery (ACoA) aneurysm is referred due to repeated recurrence despite 3 embolizations. Magnetic resonance angiography (MRA) on arrival (A) and 3-dimensional rotational angiography (B) show a thrombosed sac (asterisk) in (A) and recurrent aneurysmal sac (asterisk) in (B) involving both sides of the anterior cerebral artery (ACA) A2 opening. MRA 1-day post-procedure (C) shows complete embolization of the aneurysm sac. Note a compensatory enlargement of the right ACA A1 (thick arrow) in (C) compared with the previous ACA A1 (thin arrow) in (A). Concept diagram of the procedure (D–F). A stent is deployed in the left ACA A1–2 segment to cover the wide aneurysm neck extending toward the left ACA A2 segment. The coils are densely packed to fill the neck, and a slight protrusion toward the ACoA is intentionally allowed. The diameter of the right ACA A1 segment increases to compensate for the diminished ACoA flow from the left ACA (thin and thick arrows in [D–F]).
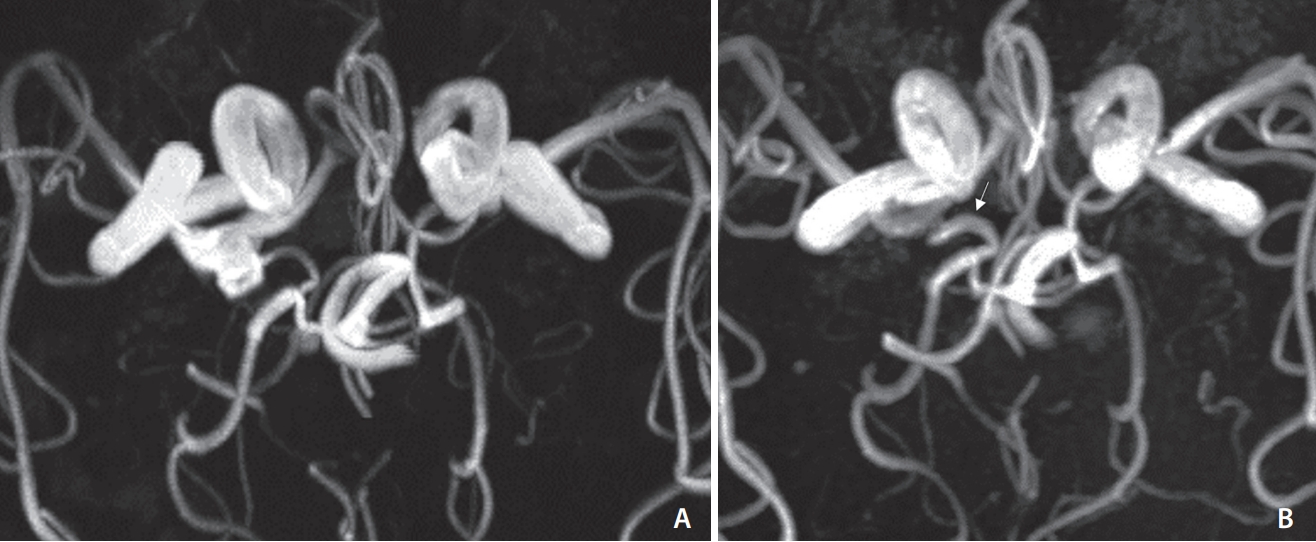
An adolescent patient (patient 9) presents with a giant aneurysm at the tip of the basilar artery (basilar tip) involving the left posterior cerebral artery (PCA) P1. Initial computed tomography angiography (A) shows a giant aneurysm sac (asterisk) that displaces the PCA arising from the aneurysm (arrow). Note that the left posterior communicating artery (PCoA) is invisible on (A) and on magnetic resonance angiography (MRA) (B) 1 day after coil embolization via the basilar artery. The 2-month follow-up MRA (C) reveals enlargement of the left PCoA and filling of a recurrent aneurysm sac (arrow) from the PCA without filling from the basilar artery suggesting back door opening after front door closure. Additional coiling (arrow) via the enlarged PCoA (D) shows the disappearance of the recurrent neck filling of the aneurysm (arrow in E) on MRA on the next day (E). The 2-year follow-up MRA (F) shows no recurrence of the aneurysm and remodeling of the left PCA (arrow), that is, physiologic flow diversion through the circle of Willis, which has a preventive effect on aneurysm recurrence at the basilar artery tip (front door).
Procedure
All endovascular procedures were performed under general anesthesia. All patients were pretreated with 100-mg aspirin and 75-mg clopidogrel daily for 5 days before the procedure. If the P2Y12 reaction unit value indicated that the patient was resistant to clopidogrel, tailored medication with low-dose prasugrel was used instead [18-20]. During the procedure, each patient received 70 IU/kg of intravenous heparin to attain an activated clotting time of approximately 250–300 seconds, as previously described. Additional heparin at 1,000 IU per hour was administered to maintain the activated clotting time. Physiologic flow diversion was applied to aneurysms at the ACoA, PCoA, or the basilar tip if they had a wide neck (defined as dome-to-neck ratio <2 or neck length >4 mm) and asymmetric bidirectional inflow from the CoW (defined as more than 10% in diameter difference of the 2 related vessels in the CoW) [9]. For the treatment of an aneurysm having a wide neck, stent-assisted coiling might be considered. Patients who underwent coiling received aspirin for 1 month after the procedure. We prescribed a 3-month course of dual antiplatelet agents or prasugrel followed by additional 3-month aspirin monotherapy if a stent was used.
Outcome Analysis
Outcome analysis included embolization status, PD, adverse event, pre and post mRS, and the presence of recurrence. Embolization status was evaluated by 1-day MRA with diffusion weighted imaging. We categorized the initial results of embolization as having complete occlusion, residual neck, and residual aneurysm. AngioCalc software (available at https://www.angiocalc.com) was used for the calculation of aneurysm volume and PD after embolization. An adverse event was defined as any clinical adverse event related to a neurological deficit (transient ischemic attack and minor or major stroke). Patient status included pre-mRS before the procedure and post-mRS evaluated at 1-day post-procedure, discharge, 1–3 months post-procedure, every year, and then at the final follow-up period.
Recurrence was evaluated using follow-up MRA. Residual or recurrent aneurysms were determined with a 3-dimensional rotational display of time-of-flight (TOF) MRA as well as the source images for TOF MRA [16-18,21-23]. A residual sac was defined as a flow-related signal in an aneurysm on TOF MRA that corresponded to a residual sac on final angiography. Aneurysm recurrence was defined as a TOF signal located in another part of the aneurysm or larger than the original signal on final angiography. Nondominant artery enlargement was defined as flow-related signal enhancement in the nondominant artery compared with pre-procedural MRA. If preprocedural MRA was not available, computed tomography angiography (CTA) was used instead. Two neurointerventionists independently decided whether the interval changes in the nondominant artery were demonstrated. If there was a disagreement, an additional neurointerventionist joined the discussion to establish a consensus.
RESULTS
The aneurysm characteristics and outcomes are presented in Table 1. Fifteen aneurysms of 14 patients were included in this study. The mean age at the time of the procedure was 58 years (range 15–75 years). A total of 10 patients (71%) were women. Four aneurysms were initially presented as recurrent aneurysms on arrival. All aneurysms had a wide neck and asymmetric bidirectional inflow through the CoW. The mean largest diameter (LD) of all aneurysms was 9.0 mm.
Five aneurysms (33.3%) underwent stent-assisted coil embolization. The mean PD of all aneurysms was 45.1%. The results of embolization status were complete occlusion in 12 aneurysms (80%) and residual neck in 3 aneurysms (20%). The mean clinical follow-up duration of all patients was 12.5 months (range of 6–40 months). The mean image follow-up duration of all patients was 12.4 months (range of 6–40 months). In follow-up MRA, remodeling of the CoW was found in 8 patients (53.3%): 5 aneurysms in ACoA (Figs. 1, 3), 1 aneurysm in PCoA (Fig. 4), and 2 aneurysms in the basilar tip (Fig. 2). No patients had neurological symptoms or radiological evidence of cerebral ischemia after coil embolization. There were no changes in the mRS in all cases between pre-procedure and post-procedure and at the last follow-up. One case (patient 14) was initially presented as mRS 1 due to Parkinsonism. There were no recurrences during the follow-up period.
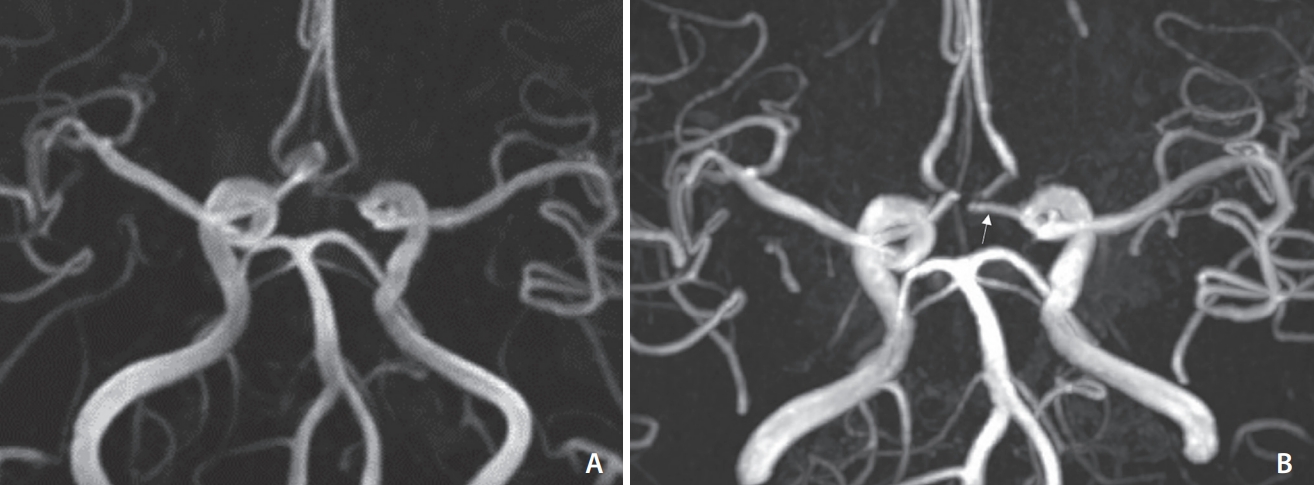
A wide-necked aneurysm (patient 5) at the anterior communicating artery (ACoA) origin of the right anterior cerebral artery (ACA). (A) Pre-embolization and (B) post-embolization magnetic resonance angiography after coil embolization with a guidewire protection technique with sufficient coiling of the neck into the ACoA. Note obliteration of the aneurysm and enlargement of the left ACA A1 after coiling as a sign of physiologic flow diversion (arrow) in (B).
A wide-necked aneurysm (patient 13) at the posterior communicating artery (PCoA) origin of the right internal carotid artery. (A) Pre-embolization and (B) post-embolization magnetic resonance angiography after stent-assisted coil embolization with sufficient coiling of the neck into PCoA. Note obliteration of the aneurysm sac and enlargement of the right PCoA after coiling as a sign of physiologic flow diversion (arrow) in (B).
Two Instructive Cases
Case 1
An adult patient with a giant thrombosed ACoA aneurysm was referred to our institution due to repeated recurrences. The patient had undergone coil embolization 3 times at an outside hospital (1 and 8 months after the coil embolization). MRA and transfemoral cerebral angiography (TFCA) on arrival showed both a thrombosed and recurrent aneurysmal sac (Fig. 1A). The LD of the thrombosed aneurysm was 40.4 mm. The left dominant ACA A1 and right nondominant aneurysms are shown. The recurrent sac was located at the ACoA origin of the left ACA and incorporated the early bifurcation site of the callosomarginal and pericallosal arteries. The bidirectional inflow in a communicating part of the recurrent aneurysmal sac was depicted in 3-dimensional rotational angiography (Fig. 1B). After discussion, the concept of physiologic flow diversion was applied to prevent further recurrence. The stent was placed across the left ACA A1 and A2 (Fig. 1D). Dense coil packing of the aneurysm sac as well as the neck opening extended to the ACoA (Fig. 1E.). A total of 50% PD was achieved. The follow-up MRA 1-day post-procedure showed no residual sac. It also demonstrated an increased flow in the right ACA A1 due to the effect of the physiologic flow diversion (Fig. 1C, F). There were no periprocedural complications. There was no recurrence at follow-up 6-month post-procedure in our institution.
Case 2
An adolescent patient complained of severe headaches. The initial CTA showed a giant aneurysm at the tip of the basilar artery involving the left posterior cerebral artery (PCA) P1 (Fig. 2A). The LD of the giant aneurysm was 30 mm. In the preoperative TFCA, the left PCA P2 was filled through the aneurysm and the left PCoA was hypoplastic. At the first session, the aneurysm sac and left PCA P1 were densely packed with coils via the basilar artery (front door closure). The follow-up magnetic resonance (MR) study 1-day post-procedure showed no residual aneurysmal sac, especially from the basilar artery (Fig. 2B), and no evidence of cerebral ischemia. At that time, the left PCoA was not observed in the 1-day postoperative MR study. The follow-up MRA 2-month post-procedure showed an enlarged left PCoA and a small residual aneurysmal sac filled from the left PCoA (opening of the back door). There were no coil compactions and recurrent sacs from the side of the basilar artery. We considered that the recurrent sac was created by progressive enlargement of the PCoA (the aneurysm’s back door opening) after front door closure (physiologic flow diversion; Fig. 2C). The additional coil embolization was performed via the left PCoA without any complications (Fig. 2D). The follow-up MRA 2-year post-procedure showed a prominent left PCoA without a recurrent aneurysmal sac. The patient was in good condition without any neurological deficits (mRS 0) during the follow-up period.
DISCUSSION
When there is a balanced development of the CoW, ipsilateral and contralateral flows need to be considered when coiling an aneurysm in the CoW because such reciprocal flow may be a factor in recurrence. We demonstrate that such a concept can also apply to giant aneurysms, which tended to recur after treatment in 2 patients. One patient had a thrombosed giant ACoA aneurysm, which repeatedly recurred after coil embolization, and was referred to our institution. The aneurysm neck was widely involved in the ACoA, which received flow from both ACA A1 segments. Additional double stent-assisted coiling or a double flow diverter was considered, and finally, we decided to use the physiologic flow diversion technique. With single stent-assisted coiling via the dominant ACA A1, we also partially packed the ACoA to preclude the flow from the opposite ACA A1 into the aneurysm. MRA 1-day post-procedure showed no filling of any residual aneurysm and also revealed enlargement of the contralateral ACA A1, which suggested successful application of physiologic flow diversion. Although the patient still required further long-term follow-up, the short-term outcome was good. The other was a basilar tip aneurysm with neck extension to the PCA P1. Dense packing of basilar inflow first induced PCoA and PCA enlargement, which filled the aneurysm backward. Additional coil packing via the PCoA could obliterate the residual aneurysm sac filling from the backflow of the PCA. The patient was stable without any recurrence during the 3-year follow-up.
Visualization of the cerebral arteries on MRA is dependent on blood flow through the arteries. When blood flow is relatively low, its visibility on TOF MRA decreases, and diameter measurements may be underestimated due to very slow flow near the vessel wall. In addition, a small underestimation of the prevalence of collateral flow in small CoW components may be expected [24]. From a hemodynamic point of view, MRA imaging of collateral flow has advantages over conventional angiography [24]. When the collateral flow is visible on MRA, it is likely to contribute significantly to maintaining regional cerebral blood flow. In general, for morphological as well as hemodynamic (flow direction) measurements in the CoW, MRA is regarded as a valuable technique [24].
There was a report on the treatment of a fusiform anterior circulation aneurysm by remodeling the CoW with a flow diverting stent [25]. A fusiform aneurysmal ACA A1 segment as a side branch relies on vascular and hemodynamic remodeling created by flow diversion. This remodeling was supported by competing inflow from the contralateral circulation via the ACoA, and it did not result in any clinical adverse events due to the collateral supply [25]. Cagnazzo et al. [26] conducted a systematic review and meta-analysis for flow-diversion treatment of unruptured saccular ACoA aneurysms. The technical success rate was 95.5% and the rate of long-term complete or near-complete occlusion was 87.4%. The overall complication rate was 8.6%. The overall rate of flow modifications of an A2 segment or recurrent artery of Heubner was 28%. The overall rate of narrowing and occlusion of covered vessels was 11% (5 cases) and 16% (7 cases), respectively. Among them, 3 cases showed symptoms due to a slow flow in the covered A2 and the coverage of the recurrent artery of Heubner [26]. Although it seemed to be feasible and safe, the use of a flow diverting stent for ACoA aneurysms had several potential disadvantages. The risk of intraluminal thrombosis, in-stent stenosis, oversizing the stent, as well as the risk of occlusion of the jailed artery or perforator should be considered when a flow diverting stent is placed in the A1 and A2 segments [27]. Several techniques using double stents (X, T, and T stenting) for a wide-necked ACoA aneurysm have been reported. The rate of complete occlusion and procedural complication were 85.5–95.7% and 6.7–17.5%, respectively. The rate of recanalization and retreatment were 0.0–7.8% and 0.0–2.4%, respectively. Double stenting techniques seem to increase thromboembolism because of insufficient wall apposition and endothelialization [28]. In our results, we did not find any ischemic complications including perforator infarction and territorial infarction. We thought that both partial occlusion of the parent artery and the potential of CoW collateral modification may prevent these ischemic events.
The potential of CoW collaterals to increase in size may be a mechanism for the collateral arteries to adapt to hemodynamic changes. Computerized flow prediction models indicated that the ACoA is the major conduit of collateral blood supply, whereas the PCoA is presumed to be more important as a source of collateral flow in patients with a small ACoA. The ACoA and ipsilateral PCoA are the collateral pathways that the CoW can redistribute blood flow to the deprived side of the brain. Asymptomatic patients with internal carotid artery (ICA) occlusion had an increased diameter of the ACoA. The potential of the CoW to provide alternative flow routes in the case of diminished arterial flow to the brain has been known since Sir Thomas Willis first described the collateral function of the arterial anastomoses in 1664 [29]. Previous studies have suggested a protective effect of collateral flow via the PCoA or have shown that a small (<1 mm in diameter) or absent ipsilateral PCoA is correlated with the presence of low-flow infarctions in patients with ICA occlusions [30]. The development of collateral flow conductance and remodeling of collateral vessels can occur following an arterial occlusion or chronic arterial stenosis. Arteriogenesis is triggered by increased wall shear stress, leading to the activation of endothelium, monocyte invasion, and secretion of growth factors and cytokines. This process is followed by matrix digestion and the proliferation of smooth muscle cells [31].
There are some limitations to our study. First, this was a retrospective, single-center study. So, cautious interpretation of the data is needed. Second, there was no long-term follow-up in some patients. Further long-term follow-up is required to confirm the endurance of the effect to prevent a recurrence. Third, a comparison study with other devices and materials was not done. The recent development of new devices or techniques can provide other solutions [32-35]. Fourth, the application of this concept is limited only to some cases in which the contralateral part of the CoW is patent even though it is hypoplastic and non-dominant. In the case of aplasia of the CoW, perfusion flow into the cerebral artery from the dominant artery can be compromised and, thus, prohibits generous dense packing from the aneurysm neck into the communicating part.
CONCLUSION
We described the concept of the physiologic flow diversion embolization technique and its application for widenecked aneurysms in the CoW. In our patients, there were no procedural complications or recurrence. This embolization technique can be used to perform dense coil packing, avoid inadvertent cerebral ischemia, and prevent a recurrence.
Notes
Fund
This work was supported by a grant from the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2018R1A2B6003143).
Ethics Statement
This study was approved by the Institutional Review Board at Asan Medical Center (IRB no. 2021-1102). Waiver of informed consent to participate was approved by the Institutional Review Board at Asan Medical Center (IRB no. 2021-1102) due to minimal risk to subjects and the retrospective nature of this study. De-identification of described cases and figures was performed. All patients whose cases or figures were demonstrated in this study consented to publish verbally and provided us with written consent for publication.
Conflicts of Interest
DCS has been the Editor-in-Chief of the Neurointervention since 2018. No potential conflict of interest relevant to this article was reported. YS has been the Assistant Editor of the Neurointervention since 2019. No potential conflict of interest relevant to this article was reported. No other authors have any conflict of interest to disclose.
Author Contributions
Concept and design: DCS. Analysis and interpretation: BK, YHC, and YS. Data collection: BK, YHC, and DCS. Writing the article: BK and YS. Critical revision of the article: BK, YS, and DCS. Final approval of the article: DCS. Statistical analysis: BK and YHC. Obtained funding: DCS. Overall responsibility: DCS.

