|
 |
- Search
| Neurointervention > Volume 6(2); 2011 > Article |
|
Abstract
Transvenous coil embolization has been successfully applied for the treatment of cavernous sinus dural arteriovenous fistula (CSDAVF). Unfortunately, the technique cannot be applied in cases of poor or absent inferior petrosal sinus or facial venous access route to the fistula. Recently, we experienced a successful embolization using direct superior ophthalmic vein approach in cases of CSDAVF which were no opacification of inferior petrosal sinus or facial vein.
Dural Arteriovenous Fistula (DAVF) refers to the abnormal direct connection between veins and arteries in the dura mater and accounts for 10-15% of all intracranial arteriovenous malformations [1]. Compared with the transverse-sigmoid sinus as the most frequent site of occurrence in western countries, the cavernous sinus is the most common location of DAVF in Asians [2]. Treatments of DAVF include manual compression of ipsilateral common carotid artery, radiation therapy, surgery, and endovascular embolization. Treatment methods of cavernous sinus DAVF (CSDAVF) may vary depending on the severity of the symptoms and type of venous drainage, but recently, transvenous embolization has been selected as the primary treatment method when applicable due to its high success rate and safety [3,, 4]. Transvenous embolization can be performed in the femoral vein or the superior ophthalmic vein. Transfemoral venous access reaches the cavernous sinus through the inferior petrosal sinus, which carries the simplest, safest and therefore preferred over the direct superior ophthalmic vein approach. However, when not accessible through the inferior petrosal sinus, direct access through the superior ophthalmic vein can be attempted. Recently, we experienced a successful embolization using direct superior ophthalmic vein approach in a case of CSDAVF which was no opacification of inferior petrosal sinus or facial vein. We describe our technique and results of treatment.
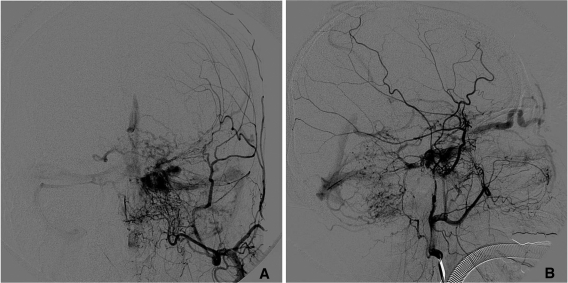
A 69-year-old woman presented with a 4-month history of diplopia, 2 months of conjuntival injection, and exophthalmos. Neurological examination showed normal consciousness and no cranial nerve deficits were observed. Magnetic resonance imaging (MRI) showed bulging of left cavernous sinus with internal signal void and distension of left superior ophthalmic vein. An angiogram showed left CSDAVF with arterial supplies from the middle meningeal artery and sphenopalatine artery arising both external carotid arteries and meningohypophyseal trunk arising both internal carotid arteries (ICAs). There was venous drainage from the anterior cavernous sinus into the left superior ophthalmic vein (Fig. 1A, B). However, angiogram did not show both the inferior petrosal sinus and facial vein, which are the typical access routes for transvenous embolization. Therefore, transvenous embolization through direct superior ophthalmic vein approach was performed.
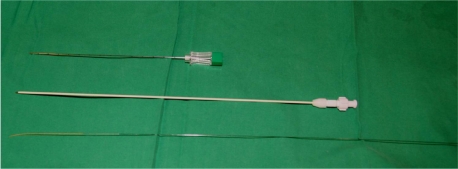
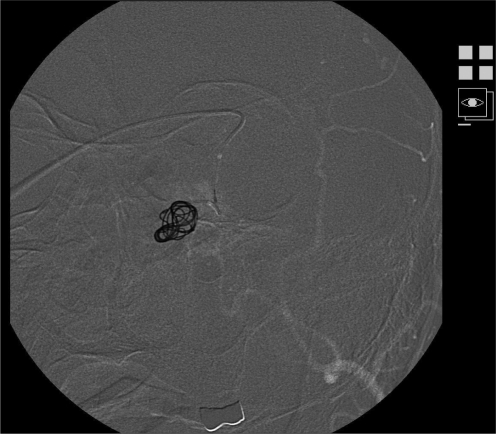
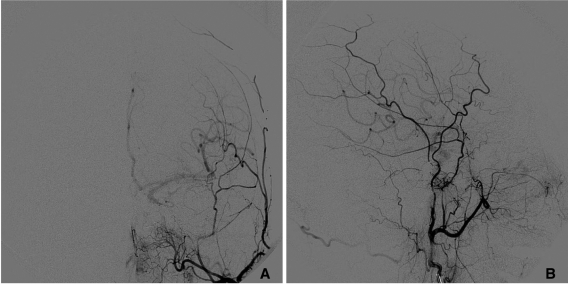
The procedure was performed under general anesthesia. We accessed the right common femoral artery, and a 5 Fr catheter (Bern; Boston Scientific, Natick, MA, U.S.A.) was placed in the left external carotid artery. Afterwards, the left eye region was prepped in sterile fashion by plastic surgeon and exposed the left superior ophthalmic vein through incision (Fig. 2). After directly puncturing the superior ophthalmic vein with a 22G needle, a 4 Fr yellow sheath from the micropuncture set (Fig. 3, Cook; Bloomington, U.S.A.) was placed in the superior ophthalmic vein. After connecting 4 Fr yellow sheath and 3-way, continuous saline flushing was performed through 3-way. It was considered that both detachable and undetachable coil embolization would be needed simultaneously and a sufficiently wide microcatheter (Prowler 18; Cordis, Miami Lakes, FL, U.S.A.) and microguidewire (Synchro 14; Boston Scientific, Natick, MA, U.S.A.) were used to approach the cavernous sinus. The microcatheter was placed into cavernous sinus and a total of 10 detachable coils (GDC 10; Boston Scientific, Natick, MA, U.S.A.) and indetachable coils (Tornado coils; Cook, Bloomington, U.S.A.) were used to perform coil embolization (Fig. 4). Post-emboliozation angiogram demonstrated near complete occlusion of cavernous DAVF (Fig. 5A, B). After embolization, the patient's diplopia and exophthalmos disappeared and there were no signs of cranial nerve palsy or additional neurological deficit.
Carotid-cavernous sinus fistulas (CCFs) can be classified into two main type. Direct CCFs consist of a communication between the main trunk of the ICA and venous channels within the cavernous sinus. CSDAVF is communications between the cavernous sinus and extradural branches of internal carotid artery, external carotid artery, or both. The direct CCFs are almost caused by severe trauma or rupture of an intracavernous carotid aneurysm, and are usually characterized hemodynamically by high flow. CSDAVF usually become symptomatic spontaneously and may be characterized hemodynamically by high or, more often, low flow [5]. Compared to other type DAVF, CSDAVF is known to have favorable prognosis and spontaneous regression rate of 10-73% in the literature [6]. Consequently, an initial conservative treatment such as manual compression of ipsilateral common carotid artery can be attempted. However, in cases of rapid deterioration of eye symptoms or cortical venous drainage occurrence, urgent interventional therapy is warranted [7]. Endovascular embolization can be done transarterial or transvenous approach. Because transarterial embolization is difficult to embolize the entire supplying artery and frequent relapse, it is currently used as a main method to transvenous embolization. Transvenous embolization can be used through the femoral vein or the superior ophthalmic vein. Transfemoral venous approach reaches the cavernous sinus through inferior petrosal sinus, and is the most preferred method due to its anatomically short and straight course [8]. However, if it is inaccessible due to thrombus in the inferior petrosal sinus, treatment can be attempted through the facial vein-superior ophthalmic vein route. If the facial vein is also inaccessible, direct superior ophthalmic vein approach can be tried instead. In this case, the bilateral inferior petrosal sinus and facial vein were not opacification on angiogram, and therefore transvenous embolization through direct superior ophthalmic vein approach was performed.
Direct superior ophthalmic vein approach has an anatomically short distance to the cavernous sinus, making it easily accessible. In this case, a 4 Fr yellow sheath was placed in the superior ophthalmic vein and after connecting 4 Fr yellow sheath and 3-way, continuous saline flushing was performed through 3-way. This procedures are allowed for a stable procedure and easily adjustable control of the microcatheter and microguidewire. We used a sufficiently wide microcatheter (Prowler 18; Cordis, Miami Lakes, FL, U.S.A.) compared previous study [9]. It would make possible using both detachable and indetachable coil embolization. However, this method is reported to cause in rare instances, bleeding and infection of the access area, damage to the trochlea area and orbital sulcus, nerve damage, dural complications such as laceration and penetration, diplopia, and prolonged ocular motor dysfunction [10].
In this case, there was no complication during or post procedure and showed completed occlusion of the CSDAVF.
In conclusion, transvenous coil embolization through direct superior ophthalmic vein approach can be good in treating CSDAVF cases where accessing the inferior petrosal sinus or facial vein are difficult or impossible.
References
1. Newton TH, Cronqvist S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology 1969;93:1071-1078 .


2. Choi BS, Park JW, Kim JL, Kim SY, Park YS, Kwon HJ, et al. Treatment strategy based on multimodal management outcome of cavernous sinus dural arteriovenous fistula. Neurointervention 2011;6:6-12.



3. Kim DJ, Kim DI, Suh SH, Kim J, Lee SK, Kim EY, et al. Results of transvenous embolization of cavernous dural arteriovenous fistula: a single-center experience with emphasis on complications and management. AJNR Am J Neuroradiol 2006;27:2078-2082 .


4. Klisch J, Huppertz HJ, Spetzger U, Hetzel A, Seeger W, Schumacher M. Transvenous treatment of carotid cavernous and dural arteriovenous fistulae: results for 31 patients and review of the literature. Neurosurgery 2003;53:836-856 .


5. Miller NR, Tamargo RJ, Murphy KJ. Treatment of dural carotid-cavernous sinus fistulas using a superior ophthalmic vein approach. Techniques in Ophthalmology 2009;7:40-44.

6. Sasaki H, Nukui H, Kaneko M, Mitsuka S, Hosaka T, Kakizawa T, et al. Long-term observations in cases with spontaneous carotid-cavernous fistulas. Acta Neurochir (Wien) 1988;90:117-120 .


7. White JB, Layton KF, Evans AJ, Tong FC, Jensen ME, Kallmes DF, et al. Transorbital puncture for the treatment of cavernous sinus dural arteriovenous fistulas. AJNR Am J Neuroradiol 2007;28:1415-1417 .



8. Cheng KM, Chan CM, Cheung YL. Transvenous embolisation of dural carotid-cavernous fistulas by multiple venous routes: a series of 27 cases. Acta Neurochir (Wien) 2003;145:17-29 .


- TOOLS
-
METRICS

-
- 4 Crossref
- 5,124 View
- 74 Download
- Related articles in NI