|
 |
- Search
| Neurointervention > Volume 7(2); 2012 > Article |
|
Abstract
Purpose
Axium™ coils were developed to improve the durability of coil-embolized cerebral aneurysms by increasing packing density. The purpose of this prospective multicenter registry was to evaluate the safety and durability of Axium™ coils.
Materials and Methods
One hundred twenty-six patients with 135 aneurysms of ≤ 15 mm in size underwent coil embolization using bare platinum coils, with Axium™ coils constituting over 50% of the total coil length. Immediate and short-term follow-up results were prospectively registered and retrospectively evaluated.
Results
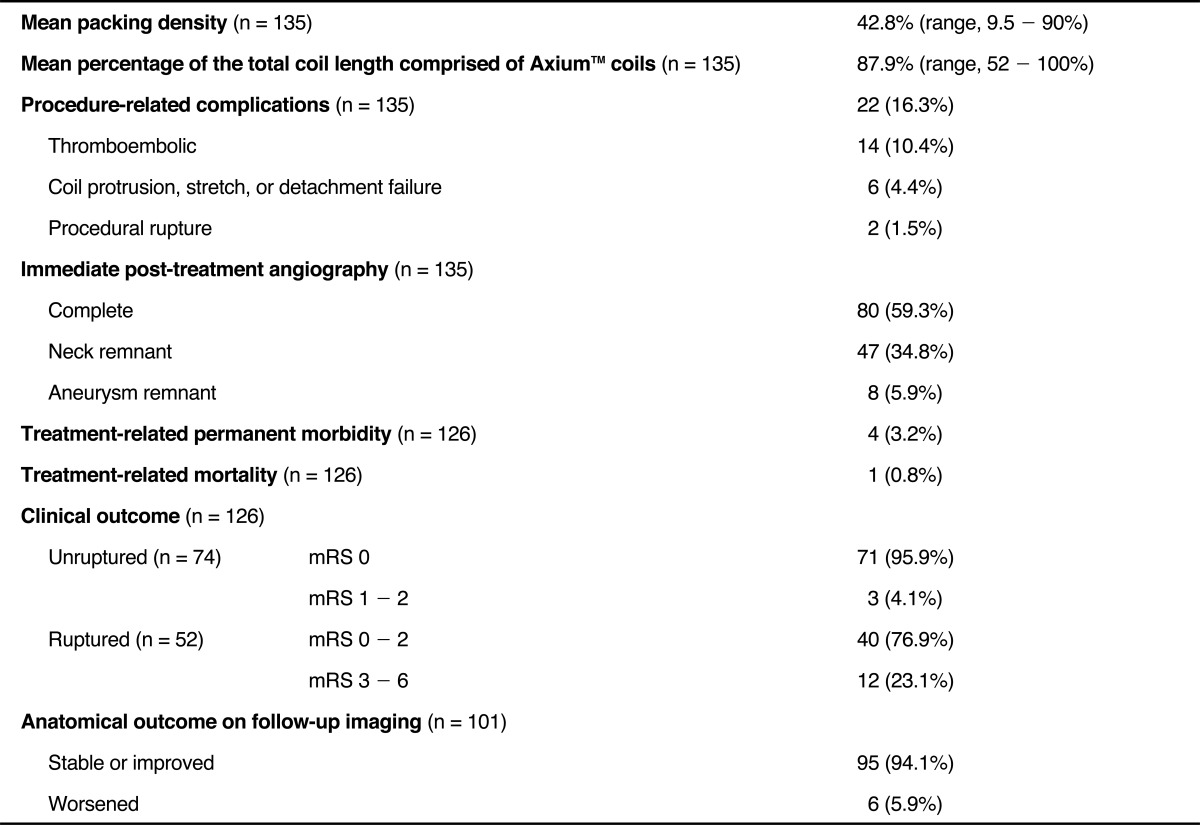
Of the 135 aneurysms (83 unruptured and 52 ruptured), immediate post-embolization angiography revealed complete occlusion in 80 aneurysms (59.3%), neck remnants in 47 (34.8%), and incomplete occlusion in 8 (5.9%). The mean packing density was 42.8% (range, 9.5 - 90%) with Axium™ coil length constituting a mean of 87.9% of total coil length. The rate of procedure-related complications was 16.3%. Procedure-related permanent morbidity and mortality rates were 3.2% and 0.8%, respectively. Follow-up catheter or MR angiography, which was available in 101 aneurysms at 6 - 15 months (mean, 7.7 months), revealed stable or improved occlusion in 95 aneurysms and worsening in 6 aneurysms (5.9%). Lower packing density (< 30%) remained the only predictor for anatomical worsening on multivariable logistic regression analysis (P < 0.05).
Conclusion
In this registry, Axium™ coils showed a relatively low rate of anatomical worsening on short-term follow-up imaging with an acceptable periprocedural safety profile compared to reports of other platinum coils. These results may warrant further study of long-term durability with Axium™ coils in larger populations.
Although coil embolization has been widely accepted both as an alternative to surgical clipping and as a primary treatment modality for intracranial aneurysms, the higher recurrence rates for coils compared to clipping remains a major limitation. To prevent coil-embolized aneurysms from recurring, various surface-modified coils have been invented and tested but, to our knowledge, have failed to prove superior to bare platinum coils in terms of durability [1,-5]. When intracranial aneurysms are treated with bare platinum coils, packing density is known to be a major factor affecting the durability of coil embolized-aneurysms [6,-8]. Axium™ coils (ev3, Irvine, CA, USA) were developed to improve the durability of coiled aneurysms by increasing packing density. The purpose of this prospective multicenter registry was to evaluate the safety, durability and packing efficacy of Axium™ coils.
The Institutional Review Board at our institution approved this prospective multicenter registry and written informed consent to treatment and data collection was obtained from all patients or their legal representatives. Inclusion criteria were 1) confirmed diagnosis of one or more intracranial aneurysms, either ruptured or unruptured; 2) aneurysm size less than 15 mm in diameter; and 3) Hunt and Hess (H/H) grade 1-4 in ruptured cases. Exclusion criteria were 1) previously treated aneurysms, 2) aneurysm associated with arteriovenous malformation or dissection, and 3) participation in a clinical investigation of another device or pharmaceutical product. The primary endpoint was an evaluation of the anatomical stability of coil-embolized aneurysms at 6 months. The secondary endpoints were 1) intra- and post-procedure safety defined as the rate of patient morbidity and mortality related to the procedure evaluated at hospital discharge and 2) aneurysm coil packing efficacy, defined as the increase in packing density which was calculated as the ratio between the volume of coils implanted and the volume of the aneurysm [coil length × π × (coil diameter/2)2] / [4π/3 × (d1/2) × (d2/2) × (d3/2)].
Between April 2008 and May 2009, 126 patients with 135 aneurysms ≤15 mm in size underwent coil embolization using bare platinum coils for which Axium™ coils constituted more than 50% of the total coil length.
The Axium™ coil consists of a bare platinum coil attached through the floating detachment link to a composite hypotube pusher, allowing rotation or bending in any direction at the detachment zone during coil insertion, and instant detachment (Fig. 1). The thickness of Axium™ coils increases from 0.0115 inches to 0.0145 inches in proportion to the increase in their shape memory diameters: 0.0115 inches for a 1.5-3 mm shape memory diameter, 0.0125 inches for 4-6 mm, 0.0135 inches for 7-10 mm, and 0.0145 inches for 12-25 mm.
Anti-platelet premedication and anticoagulation were administered at the operator's discretion and recorded. With the exception of the stent-assisted technique, any coil embolization methods including conventional single-catheter, multi-catheter, balloon-remodeling or a combination of those were permitted and were used according to the operator's preference. The stent-assisted technique was not permitted because stents have the potential to positively affect the durability of the treated aneurysms, making it difficult to evaluate Axium™ coils in terms of durability. Any type of bare platinum coils were permitted, but the Axium™ coil length had to exceed 50% of the total coil length inserted into the aneurysm sac. Any complications or adverse events during the procedure and post-procedure were recorded.
Pre-procedural evaluation included inclusion/exclusion criteria, basic demographic and patient medical history data, aneurysm characteristics, and neurological evaluation according to either modified Rankin Scale score (mRS) for unruptured aneurysms or the H/H grade at coiling for ruptured aneurysms. Post-procedural neurological evaluation was performed and recorded at 1 day post-procedure and at discharge, and any adverse events were recorded as applicable.
Clinical follow-up evaluation was performed according to each institution's standard of care. The functional neurological statuses of the patients were assessed according to the mRS and any adverse events were recorded as applicable.
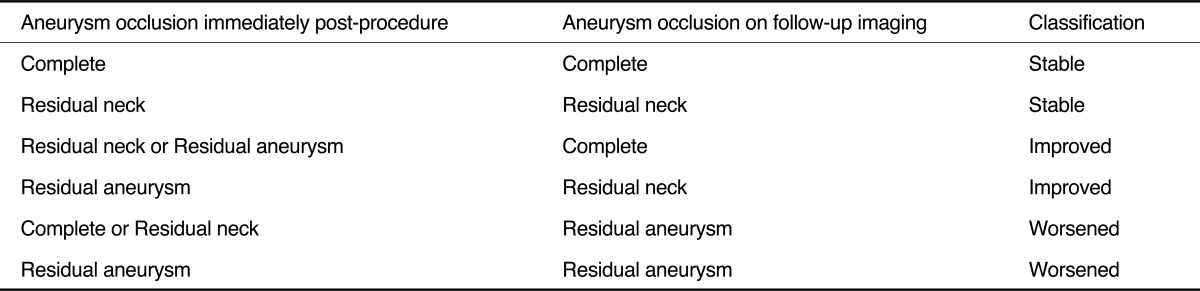
The degree of aneurysm occlusion was evaluated qualitatively according to Roy and Raymond's classification [9] immediately after the procedure. Follow-up imaging evaluation was performed either by catheter or MR angiography at 6-8 months following the procedure. The anatomic stabilities of the coil-embolized aneurysm were categorized as stable, improved, or worsened (Table 1).
All statistical analyses were performed using SPSS for Windows (version 13.0; SPSS, Chicago, IL, USA). The factors potentially affecting packing density were evaluated using a two-tailed independent t-test. Univariable analyses for presentation (ruptured versus unruptured), aneurysm location (anterior versus posterior circulation), aneurysm size (small versus large), aneurysm volume (<100 mm3 versus ≥100 mm3), neck type (narrow versus wide), embolization technique (catheter only versus balloon-assisted), and packing density (≥30% versus < 30%) were separately performed and also used to model anatomical worsening on follow-up with χ2 analysis. All variables with P < 0.25 on univariable analyses entered into a separate multivariable logistic regression analysis. The difference in packing density between the stable/improved group and the worsening group was also evaluated using a two-tailed independent t-test. Statistical significance was defined as P < 0.05 for a 95% confidence interval.
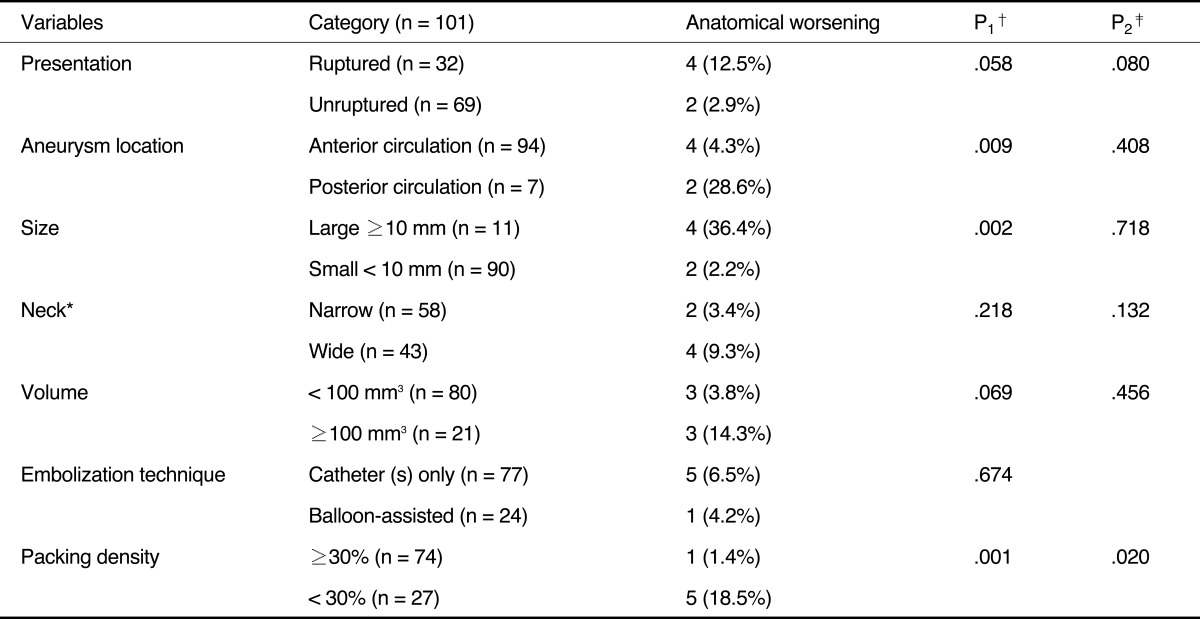
Table 2 summarizes the characteristics of the patients and the aneurysms, and Table 3 summarizes the post-treatment clinical and angiographic outcomes. Of the 135 aneurysms (mean diameter, 6 mm; 83 unruptured and 52 ruptured aneurysms), immediate post-embolization angiography revealed complete occlusion in 80 aneurysms (59.3%), neck remnants in 47 (34.8%), and incomplete occlusions in eight (5.9%). The mean coil-packing density was 42.8% (range, 9.5-90%) and the mean percentage of the total coil length inserted represented by Axium™ coils was 87.9% (range, 55.8-100%). The packing density was significantly higher in small aneurysms (44.1%) compared to larger ones (33.6%), in aneurysms with volume <100 mm3 (44.5%) compared to those with volume ≥100 mm3 group (34.0%), and in procedure using the balloon-assisted technique (47.9%) compared to the catheter(s)-only technique (40.7%) (Table 4). Use of balloon-assisted technique generally increased packing density, but the positive effects of balloon assistance on packing density were reduced with larger aneurysm volume and with wide-neck aneurysms (Figs. 2, 3). Procedure-related complications occurred in 22 cases (16.3%) and included six device-related events (coil protrusion, stretch, or detachment failure). Procedure-related permanent morbidity and mortality rates were 3.2% and 0.8%, respectively. Follow-up catheter or MR angiography, which was performed at least once in 101 aneurysms at 6-15 months (mean, 7.7 months), revealed stable or improved occlusions in 95 aneurysms and worsenned occlusion in 6 aneurysms (5.9%). There were significant differences in packing density and aneurysm volume between the stable/improved group and the anatomical worsening group (P < 0.05) (Figs. 4, 5). Posterior circulation aneurysms, large aneurysms (≥ 10 mm), and lower packing density (< 30%) were significant predictors for anatomical worsening on univariable analysis, but lower packing density (< 30%) was the only significant predictor on multivariable logistic regression analysis (P < 0.05) (Table 5).
Although coil embolization has been widely and increasingly used in current practice for treatment of both the ruptured and unruptured intracranial aneurysms, relatively higher recurrence rates after coiling remains as one of the major drawbacks of this technique [5]. For prevention of recurrence, several types of surface-modified coils have been invented but, to our knowledge, they showed no superiority to bare platinum coils in terms of durability [1,-5]. Regardless of the type of coil used, the reported recurrence rate at mean follow-up time ranging from 4.7 to 38 months was approximately 20.8% (range, 19.8-21.9% for a 95% confidence interval) with a 10.3% retreatment rate (range, 9.5-11.0% for a 95% confidence interval) [5]. Among the various factors potentially affecting aneurysm recurrence, low packing density is well known to be a predisposing factor for aneurysm recanalization [6,-8]. Axium™ detachable coils were developed to improve durability by increasing packing density.
The mean packing density in this study was 42.8%, which was superior to those found in studies using other bare platinum coils [6,-8,, 10,, 11]. Moreover, the durability of treated aneurysms on short- to mid-term follow-up was also favorably comparable to that of studies using other coils [5] Axium™ coils have two structural characteristics with respect to increasing packing density. First, the thickness of the Axium™ coils increases from 0.0115-inches to 0.0145-inches in proportion as their shape memory diameter increases. Second, floating detachment links allow rotation and bending of the coils in any direction at the detachment zone. As mentioned by Slob et al. [10] thicker coils increase packing volume per coil length per cubic millimeter of aneurysm volume. Therefore, theoretically, with an equally inserted coil length, thicker coils should lead to higher packing density. Using thicker coils especially in smaller aneurysms, however, inserted coil length can substantially be lowered to result in reducing positive effect of thicker coil on packing density. Increasing the thickness of Axium™ coils in proportion to shape memory diameter may allow the coil thickness to be appropriate for the aneurysm size and result in less resistance during coil insertion. In addition, the floating detachment link may further decrease friction, especially towards the end of the coiling procedure. As a result, these two characteristics appear to positively affect packing density as shown in the results of this study. This positive effect of Axium™ coils on packing density may explain the relatively low rate of anatomical worsening of coiled aneurysms on follow-up imaging compared with those of previous reports [5] However, the positive effect of Axium™ coils on packing density decreased similarly to other coils as the aneurysm volume increased (Fig. 1).
With regard to safety, the rates of procedure-related permanent morbidity and mortality were comparable to those of other series. Although they did not affect the clinical outcomes, device-related complications (coil protrusion, stretch, or detachment failure) occurred in six cases (4.4%). In discussion between the investigators of this study, some investigators suggested that Axium™ coils have weaker shape memory than other coils. It seemed that it was difficult to frame the initial coil basket using Axium™ coils without balloon assistance in wide-necked aneurysms.
This study has several limitations. It was not a randomized in design and therefore is susceptible to selection bias. Most aneurysms included in this registry were less than 10 mm in the largest diameter, which may increase the packing density and lower the rate of anatomical worsening on follow-up. Due to difficulty related to the multicenter registry design, Axium™ coils were not compared to a historical control group using other bare platinum coils. The limited number and period of angiographic follow-up may also lower the rate of anatomical worsening. To address this issue and to elucidate the effect of Axium™ coils on durability, further studies in larger populations with long-term follow-up period are warranted.
In this registry, Axium™ coils showed a relatively low rate of anatomical worsening on short- to mid-term follow-up imaging study with an acceptable periprocedural safety profile compared to that of other bare platinum coils reports. Further study of long-term durability of Axium™ coils in larger populations may be warranted.
References
1. Ishii A, Murayama Y, Nien YL, Yuki I, Adapon PH, Kim R, et al. Immediate and midterm outcomes of patients with cerebral aneurysms treated with Matrix1 and Matrix2 coils: a comparative analysis based on a single-center experience in 250 consecutive cases. Neurosurgery 2008;63:1071-1079 .


2. Niimi Y, Song J, Madrid M, Berenstein A. Endovascular treatment of intracranial aneurysms using Matrix coils. Early experience and midterm follow-up. Stroke 2006;37:1028-1032 .


3. Cloft HJ. HEAL investigatorsHydroCoil for endovascular aneurysm occlusion (HEAL) study: 3-6 months angiographic follow-up results. AJNR Am J Neuroradiol 2007;28:152-154 .


4. van Rooij WJ, de Gast AN, Sluzewski M. Results of 101 aneurysms treated with polyglycolic/polylactic acid microfilament Nexus coils compared with historical controls treated with standard coils. AJNR Am J Neuroradiol 2008;29:991-996 .



5. Ferns SP, Sprengers ME, van Rooij WJ, Rinkel GJ, van Rijn JC, Bipat S, et al. Coiling of intracranial aneurysms; a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009;40:e523-e529 .


6. Slob MJ, Sluzewski M, van Rooij WJ. The relation between packing and reopening in coiled intracranial aneurysms: a prospective study. Neuroradiology 2005;47:942-945 .


7. Sluzewski M, van Rooij WJ, Slob MJ, Bescos JO, Slump CH, Wijnalda D. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology 2004;231:653-658 .


8. Tamatani S, Ito Y, Abe H, Koike T, Takeuchi S, Tanaka R. Evaluation of the stability of aneurysms after embolization using detachable coils: correlation between stability of aneurysms and embolized volume of aneurysms. AJNR Am J Neuroradiol 2002;23:762-767 .


9. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke 2001;32:1998-2004 .


10. Slob MJ, van Rooij WJ, Sluzewski M. Coil thickness and packing of cerebral aneurysms: a comparative study of two types of coils. AJNR Am J Neuroradiol 2004;26:901-903 .
Fig. 1
Detachment zone of Axium™ coil. The Axium™ coil rotates and bends in any direction at the detachment zone.

Fig. 2
Relationship between aneurysm volume and packing density.
vol, volume; txmethod, treatment method
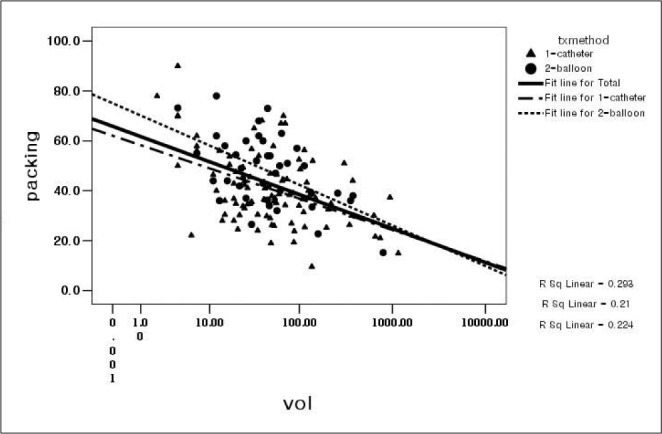
Fig. 3
Comparison of aneurysm packing densities according to coiling technique and aneurysm neck type.
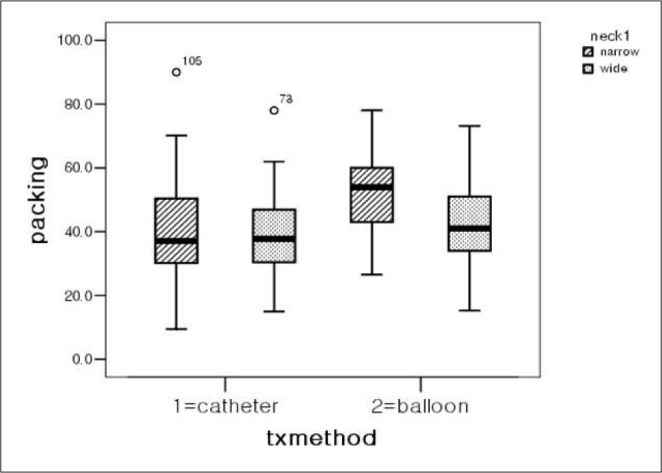
Fig. 4
Comparison of mean packing densities between the improved/stable group (no recur) and the worsening group (recur) on follow-up imaging study (p < 0.05).

Fig. 5
Comparison of aneurysm volume between the improved/stable group and the worsening group on follow-up imaging study (p < 0.05).

- TOOLS
-
METRICS

-
- 9 Crossref
- 5,332 View
- 56 Download
- Related articles in NI