INTRODUCTION
Since 2015, endovascular thrombectomy (EVT) has become the standard treatment in appropriately selected patients with acute ischemic stroke (AIS) and large vessel occlusion (LVO) [
1,
2], associated with intravenous thrombolysis (IVT), when indicated.
However, a considerable number of patients does not achieve near-complete or complete recanalization, defined as a “modified Thrombolysis in Cerebral Infarction” (mTICI) score 2c-3 [
3,
4].
The relationship between incomplete recanalization, defined as mTICI score 0, 1 or 2a, and poor outcome is strong and clear [
1-
4]. Recently, mTICI 2b score (partial filling ≥50% of the vascular territory), originally and conventionally accepted as successful recanalization, has been independently associated with worse functional outcome compared to mTICI score 2c-3 [
5-
7].
Strategies aimed at achieving complete recanalization are therefore needed [
8,
9].
Initial observational studies reported higher rate of complete recanalization in patients receiving adjunctive intra-arterial tissue plasminogen activator (iaTPA) [
10-
12], whereas better outcome after iaTPA was demonstrated in a recent small randomized controlled trial (RCT) [
13].
However, strong evidence on indications, dose, and treatment modalities of iaTPA in ischemic stroke are lacking.
AIM
To investigate whether iaTPA, as additional treatment in patients with AIS and LVO achieving mTICI score ≤2b after EVT, improves recanalization (mTICI score 2c-3), and to evaluate the incidence of symptomatic intracranial hemorrhage (ICH).
POPULATION AND METHODS
Patients with acute anterior circulation ischemic stroke and LVO, reaching mTICI score ≤2b after at least 3 passes of EVT, or experiencing distal embolization unsuitable for EVT, were prospectively selected to receive iaTPA.
Evidence of angiographic contrast extravasation, suggesting hemorrhagic transformation already during the endovascular procedure, the use of intravenous Tenecteplase for IVT and the enrollment in any different clinical trial ongoing at our center were the main exclusion criteria. IVT with alteplase was allowed, when indicated. IVT and EVT were performed according to current guidelines [
14,
15].
In cases of persistent proximal occlusion, after at least 3 passes of aspiration and/or retriever technique, a bolus of 5 mg alteplase (up to three times, i.e., 15 mg, at 5 minutes minimum interval) was infused as close as possible to the clot. Each intra-arterial alteplase administration was followed by a new attempt of mechanical thrombectomy (aspiration or retriever, at interventionist’s discretion).
In cases of clot distalization, a bolus of 5 mg of alteplase (up to three times, i.e., 15 mg, at 5 minutes minimum interval) was administrated as close and safe as possible. Angiographic status was verified 5 minutes after every bolus; patients achieving mTICI score ≥2c reached the angiographic aim of the study and the procedure was therefore interrupted. The main safety outcome was represented by symptomatic hemorrhagic transformation, defined as such if causing an increase in National Institute of Health Stroke Scale (NIHSS) score of ≥4 points, or classifiable as parenchymal hematoma type 2 [
16]. The eventual presence of ICH was assessed through serial computed tomography scans on following days.
RESULTS
From 1st of May to 31th December 2022, 201 AIS patients with LVO were treated with EVT (and IVT when indicated), and among them 15 consecutive patients achieving mTICI score ≤2b after at least 3 passes, or experiencing distal embolization, unsuitable for further endovascular attempts, were treated according to the described iaTPA protocol, at A.O.R.N. Cardarelli. Five patients, despite achieving TICI score ≤2b, were excluded from the protocol, according to the exclusion criteria: 1 because of evidence of contrast extravasation during EVT, whereas 4 patients had been included in different clinical trials. Main clinical, radiological, therapeutic and angiographical features are summarized in
Table 1 [
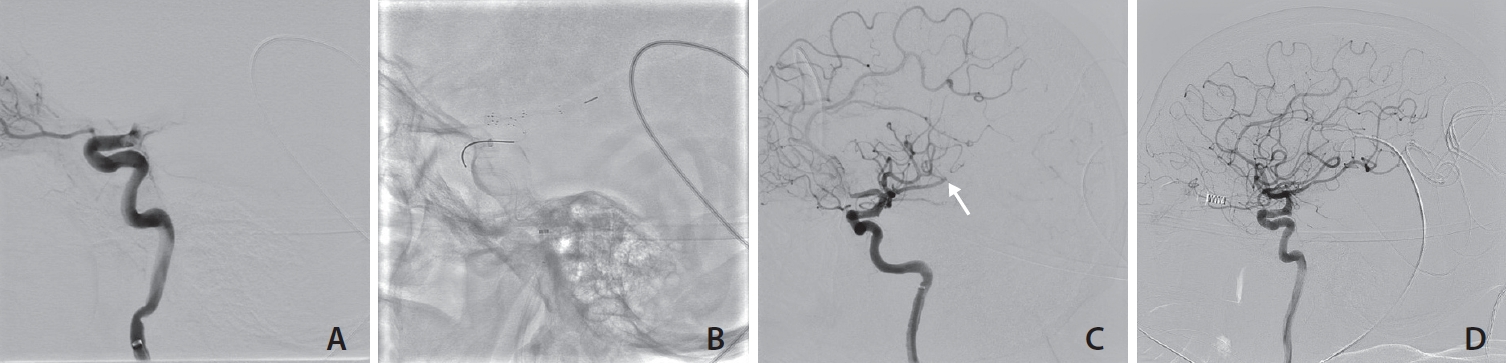
17]. IVT (0.9 mg/kg alteplase) was performed in 13 of 15 patients. Of the 2 patients who did not receive IVT, one presented beyond 9 hours after witnessed onset, and one was on Apixaban. At baseline, median NIHSS was 18, and median Alberta Stroke Program Early CT (ASPECT) score was 9. Three of 15 patients showed persistent proximal occlusion (mTICI 0-1) and 12 of 15 patients showed distal embolization (mTICI score ≥2a). 10/15 (66%) patients showed mTICI score improvement after rescue iaTPA. mTICI score ≥2c was achieved after 5 mg iaTPA in 4 patients, and after 10 mg iaTPA in 5 cases (
Fig. 1A–
D). Six of 15 patients received 15 mg iaTPA: 1 of 6 showed angiographical improvement, whereas 5 patients did not. Notably, no patients with persistent proximal (TICI ≤1) occlusion improved, even after full-dose iaTPA. However, one among these 3 patients showed delayed reperfusion confirmed on a transcranial doppler, which was performed 3 hours after EVT because of a great clinical improvement. Three patients were amenable of further endovascular attempts after iaTPA administration; 1 of 3 showed a mTICI improvement after 2 boluses and 2 thrombectomy passes, 2 of 3 received 3 boluses and 3 thrombectomy attempts, according to protocol, without any angiographic improvement.
Median NIHSS after 7 days from treatment was 3, mainly driven from successfully recanalized patients, whereas it was 16 when applicated only to patients with uncomplete recanalization. Noteworthy, no patients experienced symptomatic hemorrhagic transformation, or other major bleedings.
DISCUSSION
In this prospective case-series, iaTPA appeared to be a promising approach to pursue complete recanalization after incomplete EVT, improving angiographic results in about two thirds of treated patients. We hypothesized an empowerment of the thrombolytic effect with repeated infusions, and in most cases, angiographic improvement was detected after more than one alteplase bolus.
Rescue iaTPA appeared to be possibly more effective for residual distal occlusions, due to clot distalization or fragmentation, rather than persistent proximal occlusions. In our series, all 3 patients with persistent proximal occlusion had no effect from repeated infusion of iaTPA, up to 15 mg. However, it is interesting to note that one patient with final mTICI 1, and not amenable to thrombectomy because of hostile anatomy, showed a great clinical improvement already few hours after the procedure, suggesting a possible delayed reperfusion confirmed by a transcranial doppler.
In terms of safety, the use of additional thrombolytic could be particularly concerning in patients who had previously received full-dose 0.9 mg/kg IVT. Noteworthy, in our series, we did not find any symptomatic hemorrhagic transformation or other major bleeding, reflecting safety data from previous studies on iaTPA [
11-
13]. A previous multicentric study described the potential role of plasminogen activators in improving angiographic outcome, at a cost of a significantly higher rate of hemorrhagic transformation [
12]. However, it was burdened by great heterogeneity among the different centers in the choice of the thrombolytic drug—as some of them used urokinase—and a wide range of alteplase doses, ranging from 2 to 20 mg. Moreover, the angiographic controls were performed only at the end of the whole infusion, preventing a premature interruption in case of complete recanalization, reducing the final dose, as in our protocol.
We are aware of some issues: first of all, the dose of alteplase was chosen arbitrarily. Despite intra-arterial thrombolysis was performed for several years, before the advent of new-generation devices, there is still no consensus on the dose (fixed or tailored dose) and way of administration (bolus versus continuous infusion). Previous retrospective studies, in patients treated with EVT and iaTPA, reported doses ranging between 2 and 20 mg. A small, recent, phase 2b, RCT suggested adjunctive iaTPA at a tailored dose of 0.225 mg/kg in 15–30 minutes infusion [
12]. Our 5 minutes interval proposal relies on the drug half-life of of 3.3–6 minutes [
18], thus hypothesizing a progressively increasing thrombolytic effect.
Our report includes a small sample size, not allowing any firm conclusion. We indeed recognize there should be a strong potential bias in case series of open label interventions, and also a safety signal is highly unlikely to be observed given the low incidence of symptomatic ICH, and that any conclusion about safety is not fully reliable. In addition, the baseline characteristics of the patients indicate a heterogeneous patients’ population with mixtures of good and poor collaterals, fast and slow progressors, mild and severe strokes, and this heterogeneity further limits reliable conclusions about clinical outcome.
Nevertheless, the angiographic result, represented by the improvement in mTICI score, achieved in the majority of patients, seems very promising and it should not be underestimated, even if reported in a nonanalytic study as a case series.
We therefore emphasize the potential role of iaTPA in a specific population: those undergoing EVT who did not achieve complete or near-complete angiographic recanalization, defined as mTICI score 2c-3. It should be underlined that the target population in our study is different from that in the CHOICE trial, which included patients showing post-thrombectomy extended TICI (eTICI) score ≥2b50, with the aim of improving microcirculatory flow [
12].
The management of medium and distal vessel occlusion is debated. Most of our cases included patients with distal migration of the clot. Trials of microdevices are ongoing, but major concerns exist, such as higher risks of vessel damage. Though combined IVT+EVT improved recanalization rates, compared to EVT alone, according to recent evidence [
14], it may still be insufficient to achieve complete recanalization, due to persistent occlusions, and additional local thrombolysis may be needed.
Our case series therefore encourages the development of further studied and eventually specific RCTs, to test the effect on functional outcome of rescue-iaTPA in AIS patients with LVO, treated with EVT (with bridging IVT when indicated), who did not achieve mTICI score ≥2c.