 |
 |
- Search
| Neurointervention > Volume 16(3); 2021 > Article |
|
Abstract
Purpose
Materials and Methods
Results
Conclusion
Acknowledgments
Notes
Fund
This study was supported by the Korean Society of Interventional Neuroradiology (KSIN) research grant 2020.
Ethics Statement
This study waived approval of the institutional review board. Informed consent for publication is not required.
Conflicts of Interest
BK has been the Associate Editor of the Neurointervention since 2020. No potential conflict of interest relevant to this article was reported.
DJK has been the Associate Editor of the Neurointervention since 2018. No potential conflict of interest relevant to this article was reported.
YS has been the Assistant Editor of the Neurointervention since 2019. No potential conflict of interest relevant to this article was reported.
No other authors have any conflict of interest to disclose.
Author Contribution
Concept and design: YKI, BK, HWJ, SHS, YDW, YL, DJK, PJ, CR, SS, DSC, SSC, SHK, JSB, JR, YS, WSJ, NH, SHB, JJP, SML, JK, and WY. Analysis and interpretation: YKI, BK, HWJ, SHS, YDW, YL, DJK, PJ, CR, SS, DSC, SSC, SHK, JSB, JR, YS, WSJ , NH, SHB, JJP, SML, JK, and WY. Data collection: YKI, BK, HWJ, SHS, YDW, YL, DJK, PJ, CR, SS, DSC, SSC, SHK, JSB, JR, YS, WSJ , NH, SHB, JJP, SML, JK, and WY. Writing the article: YKI and BK. Critical revision of the article: YKI and BK. Final approval of the article: YKI. Statistical analysis: BK. Obtained funding: YKI. Overall responsibility: YKI.
Fig. 1.
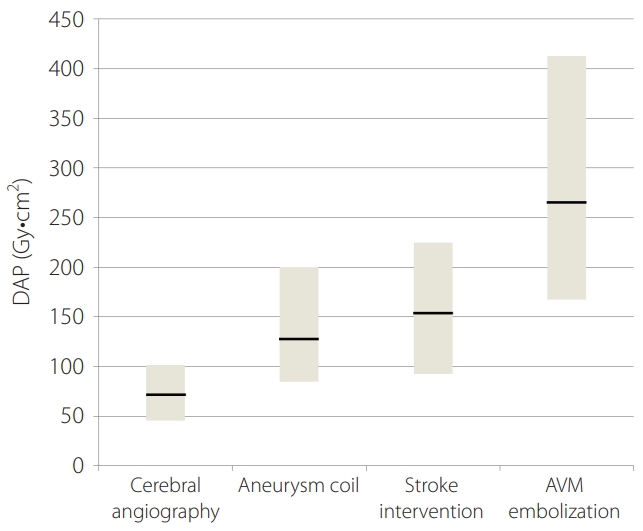
Table 1.
Table 2.
Table 3.
| Variable | Mean DAP (Gy·cm2) | AK (mGy) | FT (min) |
|---|---|---|---|
| Sex | |||
| Male (n=99) | 168.9±117 | 2,935±2,401 | 46.3±31.3 |
| Female (n=228) | 137.8±91 | 2,464±2,142 | 45.5±32.7 |
| P-value | 0.019* | 0.112 | 0.857 |
| Aneurysm location | |||
| Anterior (n=279) | 148.9±94.1 | 2,568±2,034 | 45.6±31.5 |
| Posterior (n=48) | 163.6±111.4 | 2,938±2,507 | 47.0±25.6 |
| P-value | 0.329 | 0.263 | 0.768 |
| Procedural complication | |||
| Without (n=313) | 144±86 | 2,487±1,811 | 43.3±25.0 |
| With (n=14) | 309±168 | 5,655±4,758 | 102.9±70.4 |
| P-value | 0.03* | 0.027* | 0.007* |
| Endovascular technique | |||
| Simple (S) (n=159) | 143.3±94.8 | 2,323±1,721 | 42.1±27.4 |
| Assisted (A) (n=157) | 160.7±99.7 | 2,994±2,448 | 50.6±33.9 |
| FlowDiverter (F) (n=11) | 125.5±72.1 | 1,652±522 | 30.8±11.3 |
| P-value | S vs. A: P=0.243 | S vs. A: P=0.012* | S vs. A: P=0.035* |
| S vs. F: P=0.826 | S vs. F: P=0.056 | S vs. F: P=0.459 | |
| A vs. F: P=0.472 | A vs. F: P=0.099 | A vs. F: P=0.093 |
Table 4.
Table 5.
| Variable | Mean DAP (Gy·cm2) | AK (mGy) | FT (min) |
|---|---|---|---|
| Sex | |||
| Male (n=186) | 190±124 | 1,342±948 | 33.2±25 |
| Female (n=140) | 151±116 | 1,118±892 | 36.9±29.4 |
| P-value | 0.006* | 0.04* | 0.245 |
| Occlusion site | |||
| Anterior (n=283) | 174± 114 | 1,244±883 | 34.9±26.7 |
| Posterior (n=43) | 192±146 | 1,385±1,125 | 36.0±24.3 |
| P-value | 0.345 | 0.343 | 0.799 |
| Result of recanalization | |||
| <TICI 2a (n=48) | 177±120 | 1,246±904 | 34.3±26.3 |
| ≥TICI 2b (n=278) | 170±109 | 1,358±998 | 39.8±26.2 |
| P-value | 0.725 | 0.433 | 0.178 |
| Number of device passage | |||
| 1 | 128±77 | 875±560 | 24±17 |
| 2 | 179±114 | 1,197±766 | 35±25 |
| ≥3 | 236±137 | 1,806±1,103 | 49±30 |
| P-value | 1 vs. 2: P=0.004* | 1 vs. 2: P=0.018* | 1 vs. 2: P=0.005* |
| 1 vs. ≥3: P=0.000* | 1 vs. ≥3: P=0.000* | 1 vs. ≥3: P=0.000* | |
| 2 vs. ≥3: P=0.001* | 2 vs. ≥3: P=0.000* | 2 vs. ≥3: P=0.000* | |
| Technique | |||
| Aspiration (A) | 132±118 | 866±641 | 24.3±22.5 |
| Stentriever (S) | 168±102 | 1,188±759 | 30.2±21.6 |
| Combined (C) | 208±123 | 1,558±1,067 | 45.4±28.4 |
| P-value | A vs. S: P=0.09 | A vs. S: P=0.034* | A vs. S: P=0.243 |
| A vs. C: P=0.00* | A vs. C: P=0.003* | S vs. C: P=0.000* | |
| S vs. C: P=0.019* | S vs. C: P=0.00* | A vs. C: P=0.000* |
Table 6.
Table 7.
| Variable | Mean DAP (Gy·cm2) | AK (mGy) | FT (min) |
|---|---|---|---|
| Sex | |||
| Male (n=42) | 325±199 | 4,182±3,356 | 79±51 |
| Female (n=36) | 270±162 | 3,080±2,220 | 75±49 |
| P-value | 0.195 | 0.097 | 0.757 |
| Location of AVM | |||
| Anterior (n=59) | 288±175 | 3,636±3,065 | 76±48 |
| Posterior (n=19) | 337±208 | 3,853±2,623 | 78±56 |
| P-value | 0.302 | 0.775 | 0.927 |
| Size of Nidus (cm) | |||
| <3 cm (A) | 286±175 | 3,390±2,658 | 66±42 |
| 3–6 cm (B) | 339±207 | 4,667±3,671 | 100±59 |
| >6 cm (C) | 325±233 | 3,086±2,205 | 105±62 |
| P-value | A vs. B: P=0.538 | A vs. B: P=0.242 | A vs. B: P=0.038* |
| B vs. C: P=0.992 | B vs. C: P=0.660 | B vs. C: P=0.984 | |
| A vs. C: P=0.932 | A vs. C: P=0.983 | A vs. C: P=0.376 | |
| Purpose of embolization | |||
| Preoperative (O) (n=21) | 296±167 | 2,975±1,842 | 85±52 |
| Pre radiosurgery (R) (n=21) | 193±120 | 2,396±1,424 | 47±21 |
| Curative (C) (n=36) | 364±198 | 4,826±3,613 | 92.9±55 |
| P-value | O vs. R: P=0.140 | O vs. R: P=0.774 | O vs. R: P=0.045* |
| R vs. C: P=0.002* | R vs. C: P=0.005* | R vs. C: P=0.003* | |
| O vs. C: P=0.323 | O vs. C: P=0.043* | O vs. C: P=0.843 |
Table 8.
REFERENCES
- TOOLS







